Patient Created Takeways from EULAR 2022
Our patient-led "Go With Us" team attended EULAR 2022. Here is what they think matters most to the members of our community.
Below you will find the written summary of what was discussed in the live debrief (which can also be watched on YouTube). Click on the associated video links to watch along and comment publicly on YouTube. Also check out the Glossary at the end to better understand some terms used in this overview.
Public Debrief #1 - June 23rd, 2022 led by members of the "Go With Us" team
Katie, Tiffany, Leigh, Lisa, and Eileen
EULAR 2022, Public Debrief (Part One of Two)
In this first debrief, the team focuses strongly on Personalized Therapy/Medicine, which we define as therapeutic options that are not related to pharmacologic drugs.
Watch the debrief or read the overview below!
The second Public Debrief will take place on Monday, July 18th at 11am ET/USA. REGISTER HERE to join or to receive a link to the recording.
Introduction
Every year the International Foundation for Autoimmune & Autoinflammatory Arthritis (AiArthritis for short!) attends the two largest rheumatology research conferences in the world - the American College of Rheumatology (ACR) in November and EULAR (European Alliance of Associations for Rheumatology). Attendance is vital for our organization because:
- The sessions we choose to attend provide information we need to incorporate into our own research, education, and policy efforts.
- The information we learn is about the latest advancements around the diseases we live with everyday. Helping patients learn about these, through conversations and questions/answer format, can empower patients to take more control of their own health journeys.
In this first of two debriefs, our team focused largely on the non-pharmacologic side of research, which is becoming much more popular at these conferences. Some of this research into alternative therapies is the result of the opioid/pain medication abuse crisis and a need to rethink different methods to treat pain. We also discuss newer research on early intervention, which leads to a higher chance for remission, and studies into tapering off of medications.
Can we induce drug-free remission (Debate)
Presented by Ronald van Vollenhoven, Filip van den Bosch, and Robert B.M. Landewé
This first session was chosen to review live because many of the items we wanted to cover in this debrief are mentioned at some point in this session, including: the importance to treat our diseases earlier for a higher chance of remission, tapering off of treatments, personalized and precision medicine, and the placebo and nocebo effect.
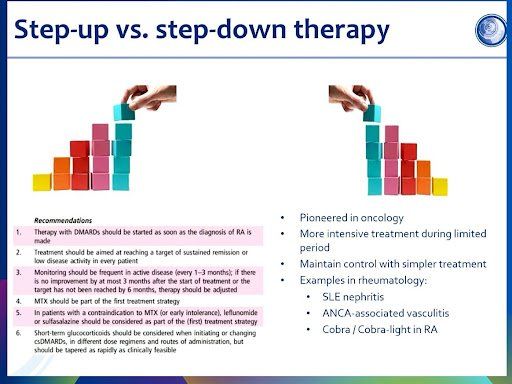
Over the past several years at both EULAR and the American College of Rheumatology (ACR) annual rheumatology conferences, we’ve seen a spike in research that focuses on remission and lasting remission. This is a result of over a decade of research that has proven treating to a target, or “Treat to Target/T2T '' early in a patient’s disease journey leads to better quality of life. (Watch/listen to Tiffany explain the history of treatments, from a pyramid approach in the early 2000’s to targeted approaches in the 2010’s to biologics first/aggressive trials, in the Public EULAR 2022 Debrief). More recently, researchers have built on this theory, conducting research testing a more aggressive approach, called “Step Down Therapy” (See photo), which starts biologic use first*. By using treatments, like biologics, first and early disease onset, data is showing some patients are achieving drug-free remission - which means some can get to a point where treatments may no longer be necessary. In this study on tapering patients with rheumatoid arthritis, all patients who achieved remission with biologics plus methotrexate therapy were then divided into three groups (biologics + methotrexate, methotrexate only, placebo/no treatment). Those continuing combination therapy, even at a reduced dose, resulted in better disease control than switching to methotrexate alone or placebo, but no significant difference was observed in radiographic progression in any of the groups. Some of the patients on no therapy (placebo) did still achieve continued remission, but only around 20% compared to 44% on the combination therapy.
In the debate, the issue of baseline (where a patient starts in their disease - mild vs severe), comorbidities, lifestyle, and other factors have to be considered to determine who realistically can be tapered off medications and have the best chances of continuing remission. Another factor to consider is, while not common, some patients only have mild disease and, therefore, it’s entirely possible they could achieve significantly improved quality of life without ever trying drugs.
Our patient panelists then discussed the importance of treating early and the time (sometimes years) it takes to find the right medication - which then decreases the chance of remission. But they also point out that with precision medicine on the horizon, there IS hope for those of us who did not get treated early, as it’s possible new research can match us to better therapies for our individual needs and, in turn, improve our quality of life significantly!
It was mentioned about other prevention studies, that take patients with genetic predisposition to developing RA (family history, certain blood markers and who have known environmental triggers, like those who smoke) and treat them with biologics prior to any onset, addressing the question, “Can we prevent RA?” Currently they could not prove it’s possible, as many of the patients still developed RA, yet it is believed onset was delayed.
AiArthritis does not believe these patients were followed over time to assess if they were able, in time, to achieve drug free remission given they were treated early and aggressively…but we’d love to know!
NOT COVERED in our debrief, but new information! From our friend and rheumatology researcher, Auralie Najm, on tapering off of medications for patients with psoriatic arthritis and axial spondyloarthritis who are in clinical remission. Check out her video report!
*The researchers do note that while the data shows the best chances for potential remission (without use of drugs anymore) did occur in people treated early and with more aggressive drugs, they understand unless guidelines would change - or unless a patient presents with very severe disease involvement near onset - it is unlikely at this time to treat this way due to healthcare system/insurance/government preferred drug plans.
How is this related to the work we do at AiArthritis?
Through our education and awareness, as well as our efforts to create patient-reported disease brochures, we are ramping up our efforts to help expedite detection, diagnosis, and access to the best therapy for each person. We understand, partly through what we learn at these conferences, that early intervention and access to the best therapy is vital to improved quality of life. We will use the information learned, in combination with our own experiences as patients, to lead efforts to ensure no one has to wait for a diagnosis or treatment.
Not Another Pill
Presented by Pernille Friis Rønne, Jo Nijs, Christine Stamatos, & Axel Finckh
Chronic pain is a complex issue that requires attention not only to the physical but to the psychological and social issues it causes, too. It also can be exhausting trying to manage self care, so integrative approaches - like lifestyle changes, coping strategies, and building support systems between family and doctors - needs to be incorporated into personalized pain management.
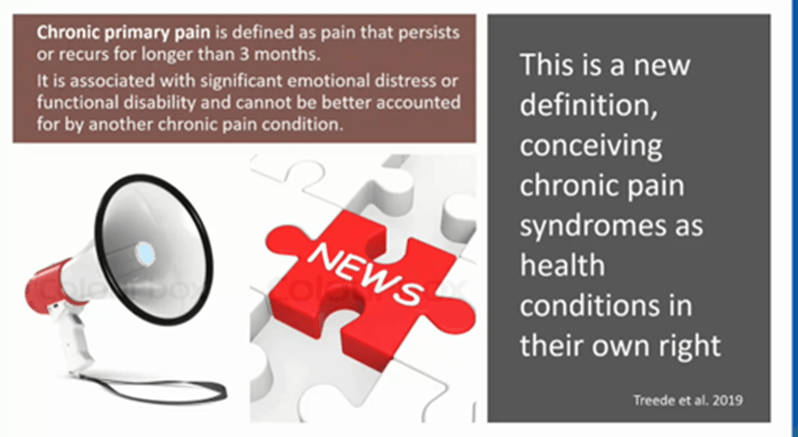
For many years standard treatments involved pharmacologic drug management, but more recently focus has been on research into treating pain with non-pharmacologic options. In the new version of the ‘master codebook’ (ICD-11), Chronic Pain will have its own code, which means it can be treated as its own condition and prescribed therapies - potentially NON-pharma options - to manage it! Additionally, doctors need to consider “Pain Anamnesis”, or the specific details and causes of pain as explained by the patient, such as debut (when it started), localization (where it’s felt), intensity (how much it hurts), type of pain (why does it hurt). Also, patients beliefs can strongly impact their physical and mental health (i.e. “I’m telling you, there is pain even if you don’t see it!”), so a support system - including being believed by your doctor - is an important step towards managing pain.
Overall, the “gold standard” for addressing pain is to combine biology, psychology, and social factors. An example of this combination - chronic stress activates what are called glial cells (in the central nervous system), increasing adrenaline and cortisol which, over time, increases inflammation (pain). So interestingly, the suggestion is to use a targeted approach (body, mind) since all of these factors of a person's life contribute to chronic pain.
How is this related to the work we do at AiArthritis?
Chronic pain is one of the most common symptoms that connects all AiArthritis diseases, but more importantly is one of the most disruptive parts of the conditions that we must manage day to day. While physical activity is often recommended to people with AiArthritis, we know that being more active is not that simple. Patients must overcome physical limitations/mobility issues, pain, and fatigue before becoming active. Patients should speak to their physical and physical therapists for exercise information.
AiArthritis
advocates for therapies that consider the individual person and their needs. We have several programs, like this
“Go With Us” to Conferences, our
AiArthritis Voices 360 Talk Show, and our
new AiArthritis research database that aim to educate and empower our fellow patients to join our research and policy efforts.
Addressing the effect of Placebo, Nocebo, and Contextual Factors in RMDs
Presented by Lene Vase, Elisa Carlino, Evrydiki Kravvariti, and Joana Vicente
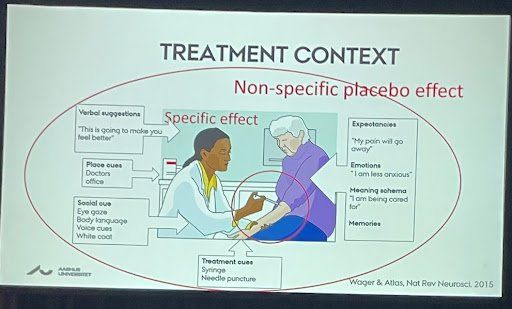
Historically, the word placebo has been used mostly in clinical trials. When new therapies are tested some of the people in the trial are on the drug, but others are given something (same method, like an injection) but it’s not the drug (could be saltwater). Those on the placebo often will report feeling better, even though they actually have received no medication. This is called a placebo effect. Nocebo is the opposite - this is when you do receive a treatment but before you do you convince yourself it’s not going to work and, thus, it does not. This phenomenon is being studied now as a potential non-pharmacologic way to manage pain.
Two studies were discussed.
The first was a pain study where patients were told, “You are getting a strong pain medication.” Within hours, the patients reported feeling better. However, they never received any medication, but rather saline water.
Another study tested patient response to biosimilars, or a newer class of drugs that are similar to the original drug but have slight differences in the non-active ingredients due to manufacturing processes. The patients who were educated on safety and efficacy studies of biosimilars, and who were able to make a choice about switching to them with their doctor, responded more positively to the drug (i.e. “it’s working!”). Whereas those not educated and forced to switch to biosimilars largely reported they were not working as well.
The concept of mindfulness and how we can use it to influence outcomes is growing. This includes both personal support as well as
understanding the chemical changes in the brain that are affected by our perceptions, negatively (associated with the nocebo effect) or positively (associated with the placebo effect). Understanding how the brain is associated with the impact on our immune responses is being explored in regards to the potential to use this phenomenon to minimize medication. While there are many ways outside influences can impact our perceptions - positively or negatively - it is largely thought that the easiest and perhaps most powerful influence can happen when there is a strong patient-doctor relationship. #lovemyrheumy
How is this related to the work we do at AiArthritis?
We know a patient's support system - which includes both their inner personal circle of friends and family, as well as their medical/therapeutic team - is a vital part of mental and physical health. That's why we have started the Supporting Me, Supporting You, Supporting Us guide for patients AND others in their support network to communicate needs and, in turn, improve relationships and support. Additionally, through our many projects around shared-decision making and our RheumyRounds talk show series, we are invested in helping improve patient-doctor relationships and patient empowerment over their health journeys.
Overview of Precision Medicine and Teaser for the Next Debrief!

The team ended the debrief by mentioning a couple additional themes that would be covered more in Debrief 2, scheduled for July 18th, at 11am ET/USA.
The first was Precision Medicine, specific to biomarkers (blood, tissue, saliva) used to help with diagnosis, matching patients to the best treatment for their individual needs, and identifying potential negative side effects based on a persons biology. Research on biomarkers and looking into disease subgroups was EVERYWHERE! Some diseases included psoriatic arthritis, lupus, rheumatoid arthritis, sjogren's syndrome, spondyloarthritis, juvenile arthritis, Still's Disease.
Another theme emerging is aging. We are the first generation of patients who may be using biologics from young adulthood through old age. Furthermore, there's a new subgroup of patients identified called "Late Onset RA (rheumatoid arthritis)", who are over the age of 65 at onset. How do we treat new elderly patients who have existing comorbidities and potential bone density issues?
Finally, subgroups and specifics- like enthesitis (the tendons, often associated with spondyloarthritis diseases like Axial Spondyloarthritis (non-radiographic/Ankylosing Spondylitis), Psoriatic Arthritis, Enthesitis-Related Arthritis.
How is this related to the work we do at AiArthritis?
Since we became a nonprofit in 2011, we have worked around the clock to solve problems that patients identify are the most important to address. Through many conversations and several projects, we have narrowed the scope of our work largely to include expedited detection and correct diagnosis, access to the best personalized (non-pharma) and precision (drugs) therapy for individualized needs, and global understanding about our diseases and the challenges associated with them. We have also become patient experts on Precision Medicine, Biomarkers, and how research can be used to influence legislation/access to therapies (pharma and non-pharma). We are launching the AiArthritis Database, under the umbrella of the FORWARD: National Data Bank for Rheumatic Diseases, where we will focus on these priorities and use the data to educate, empower, and influence healthcare needs.
Glossary of terms used:
- Anamnesis: A patient's account of a medical history
- Glial cells: Cells located in the nervous system with specific jobs to keep the brain functioning
- Placebo: Placebo historically is associated with clinical trials, when one group gets a medication and the other doesn't, but they don't know which is which (the one without medication is the placebo, or comparison group).
- Nocebo: Negative effect on a person's health as a result of negative perceptions
Want to "Go With Us?" to the next conference?
You can be a part of our "Go With Us" team!
Every year our organization attends two of the most important scientific conferences - the American College of Rheumatology (ACR) and European Alliance of Associations for Rheumatology (EULAR) Congress formerly the European League Against Rheumatism. For EULAR 2022, AiArthritis acquired passes for 16 patients from around the world to attend EULAR 2022 virtually, alongside our team of three who attended in person. Several others have joined us as 'insiders' - meaning they are not able to access and watch the sessions virtually, but they get insider videos and updates from the team attending in person. There's no other program like this, don't miss out!!! It's FREE!
Sign up for our newsletters
International Foundation for AiArthritis
6605 Nottingham Ave.
St. Louis, MO 63109-2661
Toll Free: 1-877-609-4226
Text: 1-314-282-7214
Copyright 2024. All rights reserved. Information on this site is intended for informational purposes only Our foundation does not engage in the practice of medicine. Please consult a physician to obtain personal healthcare and treatment options. 501(c) 3 Nonprofit Tax ID: 27-1214308.



