4 Patient-Care Centered Studies on IgG4-RD That You Need to Know About

IgG4-Related Disease (IgG4-RD) is a rare immune-mediated condition that can impact nearly every organ in the body. As researchers are still studying how IgG4-RD works, many new studies have emerged that examine treatments, diagnostic journeys, and outcomes for people living with IgG4-Rd.
In this post, we break down four of the most impactful and recent IgG4-RD studies on patient-centered care that provide key insight into this condition and how healthcare providers and patients cand understand and manage the diagnosis journey.
Why is AiArthritis raising awareness about IgG4-RD? Although IgG4-RD is not officially part of the AiArthritis disease umbrella, AiArthritis is raising awareness because it may end up being classified as autoimmune or autoinflammatory in the future. Additionally, as IgG4-RD is often confused with other conditions, many people with IgG4-RD may be misdiagnosed with an AiArthritis disease or face challenges getting a diagnosis.
Study That Examines Which IgG4-RD Patients Can Safely Stop Treatment and Maintain Remission
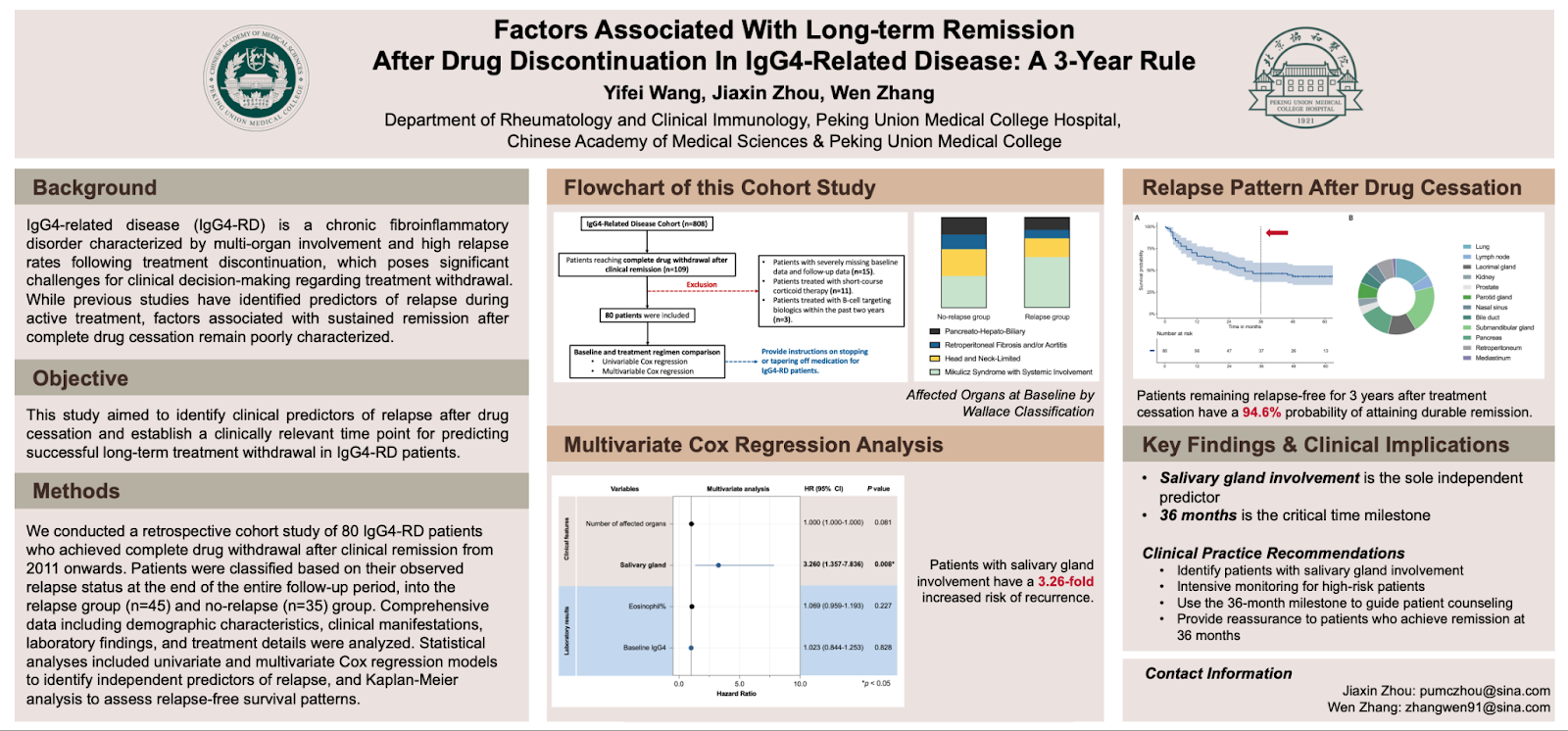
Factors Associated With Long-Term Remission After Drug Discontinuation in IgG4-Related Disease: A 3-Year Rule
Summary
This study explored which patients with IgG4-related disease (IgG4-RD) can safely stop treatment and maintain long-term remission without relapse. Since both continuing and discontinuing glucocorticoid (GC) or immunosuppressant (IM) therapy carry risks, identifying predictors of durable remission is critical. Researchers from Peking Union Medical College found that patients without salivary gland involvement and those who used an immunosuppressant early in treatment were significantly less likely to relapse after stopping medication. Additionally, remaining relapse-free for three years strongly predicted long-term remission.
Questions Answered by this Poster
- What factors predict relapse in IgG4-RD patients after treatment withdrawal?
- Does early use of immunosuppressants (IM) improve long-term outcomes?
- How long must patients remain relapse-free before remission is likely to last?
- Which organ involvements are associated with a higher risk of relapse?
Methods
- Study design: Retrospective cohort of IgG4-RD patients at Peking Union Medical College Hospital (China).
- Participants:
- 808 screened; 80 achieved remission before stopping treatment.
- Divided into: No-relapse group (n=37) and Relapse group (n=43).
- Criteria: All met 2019 ACR/EULAR classification standards for IgG4-RD.
- Data collected:
- Demographics, family history, organ involvement, lab markers, and treatment regimens.
- Laboratory values (IgG4 levels, eosinophil counts) before and after medication withdrawal.
- Statistical analyses:
- Univariate Cox regression for relapse predictors (HR, CI, p-values).
- Kaplan-Meier curve to estimate relapse-free survival over time.
Results
- Relapse group:
- More likely to have salivary gland involvement (submandibular and parotid).
- Less likely to have received immunosuppressant (IM) therapy at baseline.
- Higher baseline and pre-withdrawal IgG4 levels and eosinophil counts.
- Protective factors (lower relapse risk):
- Initial IM use → HR 0.41 (95% CI 0.20–0.84, p = 0.017).
- No salivary gland involvement → HR 3.26 (95% CI 1.32–8.06, p = 0.012).
- Time to relapse:
- Biphasic pattern with most relapses in first 36 months post-withdrawal.
- Patients relapse-free for 3 years had a 94.6% chance of long-term remission.
Conclusions
IgG4-RD patients without salivary gland involvement and those who begin treatment with immunosuppressants have a significantly lower risk of relapse after stopping therapy. The study suggests that three years of relapse-free status can serve as a practical clinical marker for durable remission, helping physicians tailor follow-up and maintenance strategies more effectively.
Key Data
- Sample: 80 remission patients (37 no-relapse, 43 relapse).
- Predictive markers:
- No salivary gland involvement (HR 3.26; p = 0.012).
- Initial IM therapy (HR 0.41; p = 0.017).
- Main relapse sites: Submandibular and parotid glands.
- Relapse-free 3 years = 94.6% probability of durable remission.
Authors
Yifei Wang, Yuxue Nie, Jingna Li, Jialei Zhang, Qinhuan Luo, Xinli Yang, Jialing Jiang, Nianyi Zhang, Linyi Peng, Yunyun Fei, Jiaxin Zhou, and Wen Zhang.
Affiliations: Peking Union Medical College and Peking Union Medical College Hospital, Beijing, China.
Read the published abstract in ACR Meeting Abstracts
Study Highlights the Importance of Early Diagnosis and Treatment for IgG4-RD
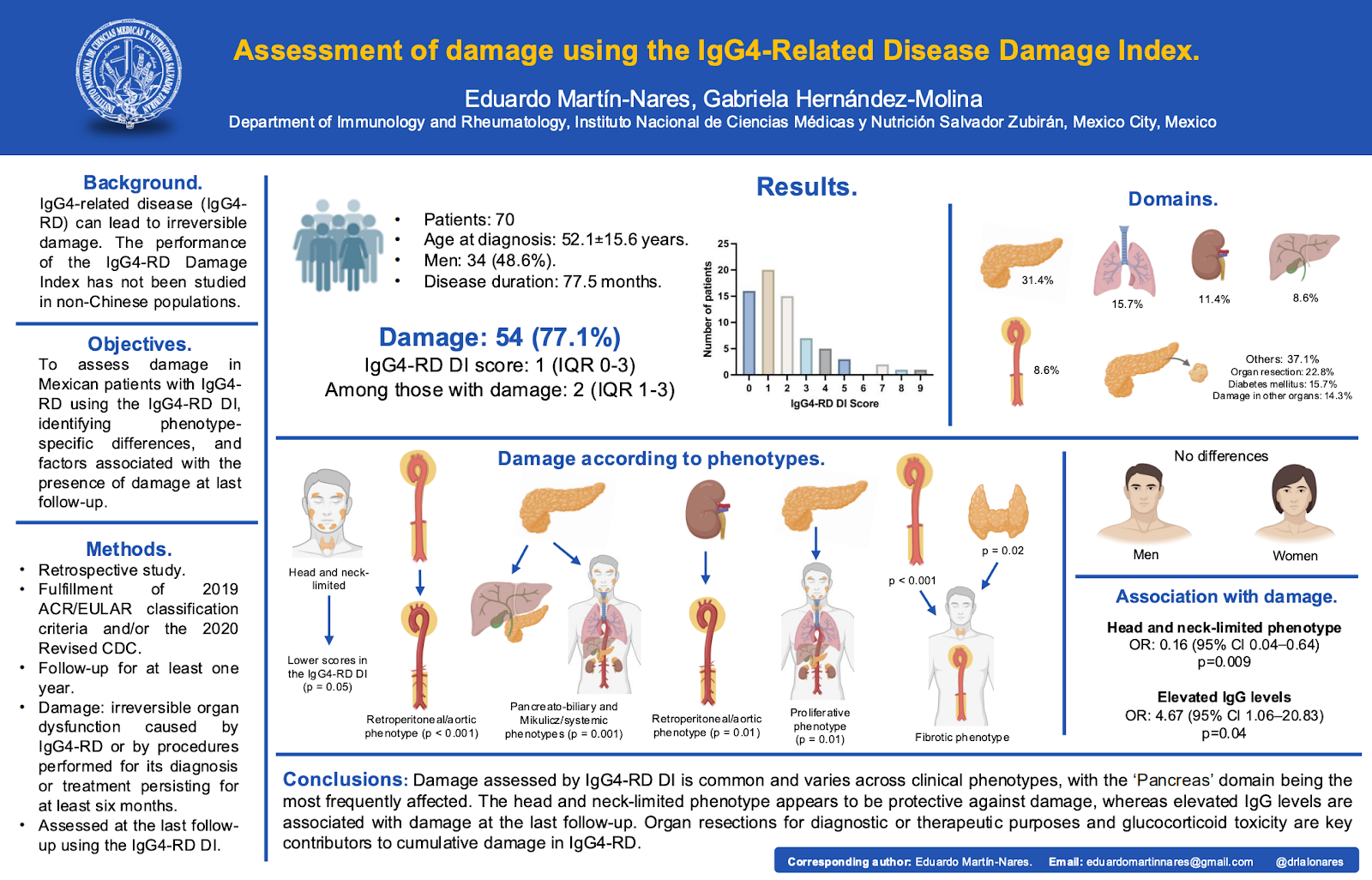
Assessment of Damage Using the IgG4-Related Disease Damage Index
Summary
This study evaluated how often and where permanent organ damage occurs in patients with IgG4-related disease (IgG4-RD) and how the IgG4-RD Damage Index (DI) performs in a non-Chinese population. Researchers from Mexico found that organ damage was common (80%), especially in the pancreas, lungs, kidneys, and retroperitoneum, and that damage patterns differed by disease phenotype. The study highlights the importance of early diagnosis and careful management to prevent irreversible organ complications.
Questions Answered by this Poster
- How common is permanent organ damage in IgG4-RD?
- Which organs are most often affected by irreversible damage?
- Do certain disease types or phenotypes carry higher or lower damage risk?
- Can the IgG4-RD Damage Index (DI) effectively measure and compare damage across patients?
Methods
- Study design: Retrospective analysis at the Instituto Nacional de Ciencias Médicas y Nutrición (Mexico).
- Participants: 70 patients meeting 2020 Revised Comprehensive Diagnostic Criteria and/or 2019 ACR/EULAR Classification Criteria for IgG4-RD.
- Follow-up period: ≥1 year.
- Damage definition: Irreversible organ dysfunction caused by IgG4-RD or by its diagnostic/treatment procedures, persisting ≥6 months.
- Assessment: IgG4-RD Damage Index (DI) scored at last follow-up.
- Analysis: Comparisons by phenotype, organ domain, and clinical characteristics (IgG levels, complement levels, remission/relapse status).
Results
- Damage prevalence:
- 56 of 70 patients (80%) had organ damage.
- Median DI score = 1 (IQR 0–3).
- Among those with damage: DI median = 2 (range 1–9).
- Most commonly damaged organs:
- Pancreas (31.4%)
- Lung (15.7%)
- Kidney (11.4%)
- Retroperitoneum/Mediastinum (8.6%)
- Liver/Biliary tree (8.6%)
- Key associations:
- High IgG levels were linked to greater damage (60.9% vs. 31.3%; p = 0.04).
- Head and neck-limited phenotype had the least damage (20.4% vs. 56.3%; p = 0.005).
- Fibrotic subtype often showed retroperitoneal or thyroid damage, while proliferative subtype showed pancreatic damage.
- Additional contributors to damage:
- Organ resections (22.8%)
- Disease- or treatment-related diabetes (15.7%)
- Glucocorticoid toxicity and diagnostic procedures
Conclusions
Organ damage is frequent and varies by phenotype in IgG4-RD. The pancreas is the most affected organ, and patients with higher total IgG levels face a greater risk of irreversible damage. Conversely, those with head and neck-limited disease tend to experience less damage. These findings support using the IgG4-RD Damage Index (DI) to monitor disease progression and tailor treatment to minimize long-term harm.
Key Data
- Patients with damage: 56/70 (80%)
- Median DI score: 2 (range 1–9)
- Most affected organs: Pancreas → 31.4%, Lung → 15.7%, Kidney → 11.4%
- High IgG linked to damage: p = 0.04
- Head/neck-limited phenotype protective: p = 0.005
Authors
Eduardo Martin-Nares and Gabriela Hernández-Molina,
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico.
Read the published abstract in ACR Meeting Abstracts
Study Exploring When IgG4-RD Patients Should Start Treatment
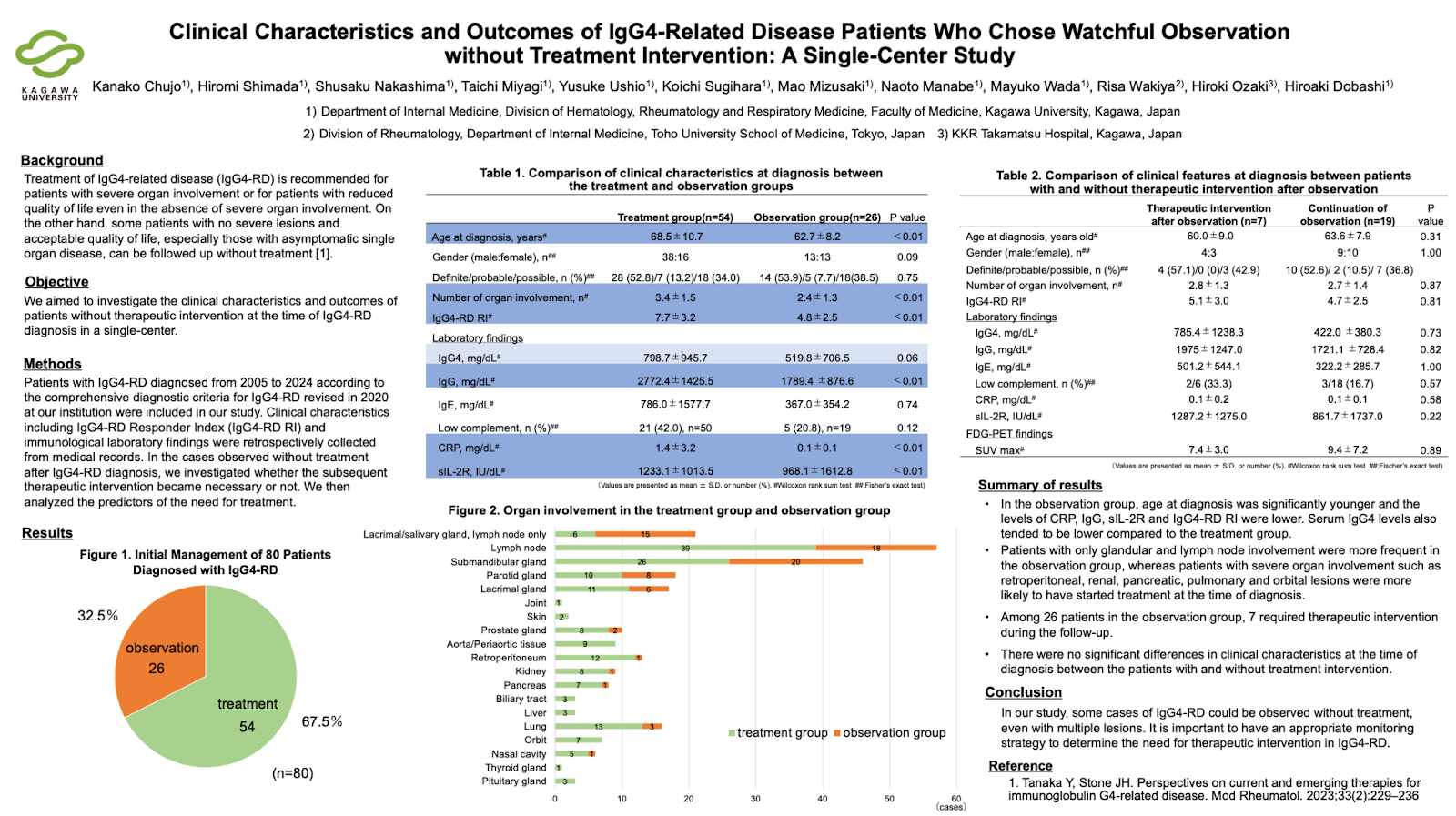
Clinical Characteristics and Outcomes of IgG4-Related Disease Patients Who Chose Watchful Observation Without Treatment Intervention: A Single-Center Study
Summary
This study explored when treatment is needed for people newly diagnosed with IgG4-related disease (IgG4-RD) and when it may be safe to observe the disease without starting medication immediately. Researchers reviewed 80 cases and found that about one-third of patients were monitored without treatment. Those patients were typically younger, had lower inflammation markers, and had milder disease—often limited to glands or lymph nodes. Over time, most remained stable, though some required treatment later when new organ involvement appeared.
Questions Answered by this Poster
- Which IgG4-RD patients can be safely monitored without starting treatment?
- What clinical or lab factors predict who might eventually need therapy?
- How do organ involvement patterns differ between treated and observed patients?
- How long can untreated patients remain stable before needing intervention?
Methods
- Study period: 2005–2024
- Setting: Kagawa University Hospital, Japan
- Participants: 80 patients diagnosed using the 2020 Revised Comprehensive Diagnostic Criteria for IgG4-RD
- Groups:
- Treatment group: 54 patients (67.5%) started therapy at diagnosis
- Observation group: 26 patients (32.5%) were monitored without treatment
- Analysis: Compared demographics, labs, and organ involvement; tracked which observed patients later required treatment and why
Results
- At diagnosis:
- Observation group was younger and had lower IgG, CRP, sIL-2R, and IgG4-RD RI scores.
- Glandular and lymph node-only disease was more common in the observation group.
- Severe organ involvement (retroperitoneal, renal, pancreatic, pulmonary, or orbital) was more frequent in patients who began treatment.
- During follow-up:
- 7 of 26 observed patients (27%) eventually required therapy.
- New organ involvement, especially pancreatic disease, triggered treatment in 5 of these 7 patients.
- Average time to treatment: 30 ± 25 months after diagnosis.
- No significant baseline differences predicted who would later need treatment.
- 19 patients (73%) continued observation without needing medication, even with multiple organ involvement.
Conclusions
Many IgG4-RD patients—especially those with limited glandular or lymph node disease and low inflammation—can be safely monitored without immediate treatment. However, regular follow-up is essential, as some patients may develop new organ involvement that requires timely intervention.
Key Data
- Total patients: 80
- Treatment at diagnosis – 54 (67.5%)
- Observation only – 26 (32.5%)
- Observation group characteristics:
- Younger (average age ~63 years vs. 69 years in treatment group)
- Lower inflammation (CRP 0.1 vs. 1.4 mg/dL)
- Lower IgG levels (1789 vs. 2772 mg/dL)
- Lower disease activity (IgG4-RD RI 4.8 vs. 7.7)
- Commonly affected organs:
- Observation group – glands (lacrimal, salivary, lymph nodes)
- Treatment group – kidneys, lungs, pancreas, retroperitoneum, orbits
- Of the 26 observed:
- 7 required later treatment (27%)
- 19 remained stable without therapy (73%)
Authors
Kanako Chujo, Hiromi Shimada, Shusaku Nakashima, Taichi Miyagi, Koichi Sugihara, Yusuke Ushio, Mao Mizusaki, Naoto Manabe, Mayuko Wada, Risa Wakiya, Hiroki Ozaki, Hiroaki Dobashi
Affiliations: Kagawa University and Toho University School of Medicine, Japan
Read the published abstract in ACR Meeting Abstracts
Study Highlights the Challenges, Frequent Misdiagnoses, and Daily Impact that IgG4-RD Patients Face
Diagnostic Journey, Clinical Burden, and Quality of Life of Patients with IgG4-RD: Results of a Cross-Sectional Survey of Patients and Physicians in the United States
Summary
This study describes the real-world experiences of people living with IgG4-related disease (IgG4-RD) in the United States. It highlights how long it takes for patients to be diagnosed, which symptoms and organs are most commonly involved, what treatments are used, and how the disease affects quality of life. Overall, the findings show that IgG4-RD is often misdiagnosed at first, requires many tests and doctor visits, and has a meaningful impact on day-to-day function.
Questions Answered by this Poster
- What does the average diagnostic journey look like for IgG4-RD?
- Which symptoms and organs are most commonly affected?
- Who typically manages IgG4-RD care?
- What treatments are being used in real-world practice?
- How does IgG4-RD impact fatigue, daily activities, and work?
Methods
- Data came from the Adelphi IgG4-RD Disease Specific Programme™, a U.S. survey conducted in 2023–2024.
- Physicians submitted detailed information on 161 patients with IgG4-RD.
- 27 patients completed questionnaires on fatigue, quality of life, and work impact.
- Information collected included:
- Symptoms at first presentation
- Organ involvement
- Diagnostic tests and number of consultations
- Treatments used and timing
- Hospitalizations
- Patient-reported outcomes (FACIT-Fatigue, EQ-5D-5L, WPAI)
Results
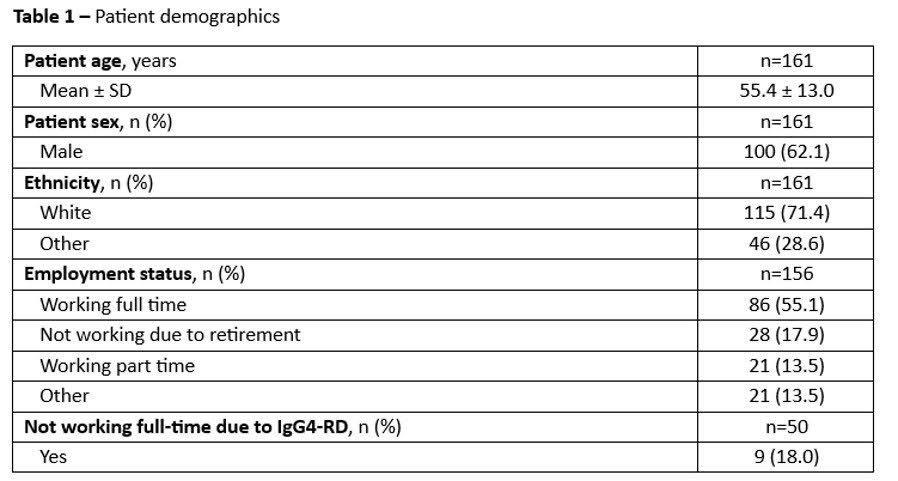
- Participants: 161 physician-reported patients; 27 completed surveys. Average age 55; 62% male; 71% White.
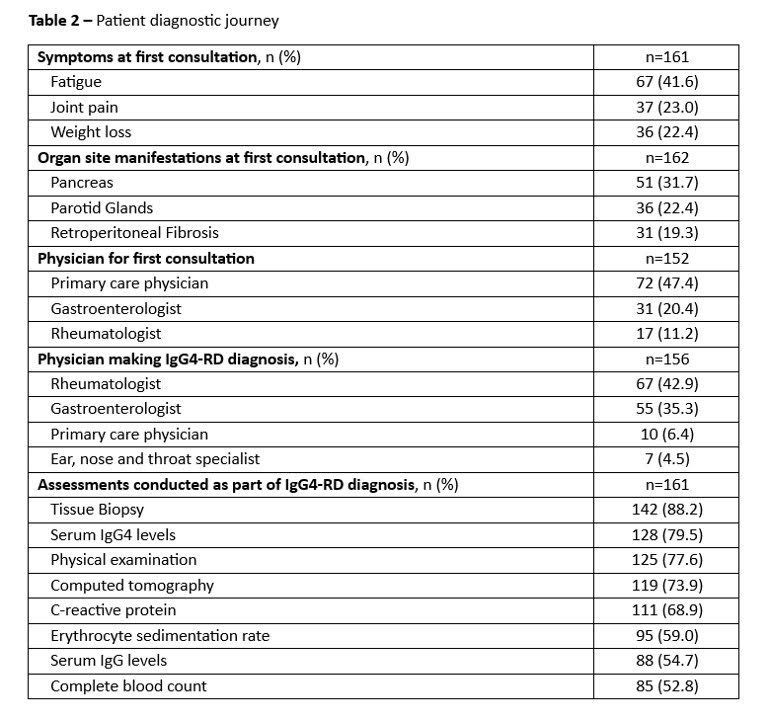
- Before diagnosis: Symptoms began around age 50. Diagnosis took ~11.5 months. Most common initial symptoms were fatigue (42%), joint pain (23%), and weight loss (22%).
- Organ involvement: Pancreas (32%), parotid glands (22%), and retroperitoneal fibrosis (19%) were most affected.
- Diagnostic journey: First evaluations were usually by primary care (47%), gastroenterology (20%), or rheumatology (11%). Patients saw ~3 providers and underwent ~13 tests. 90% were initially misdiagnosed (often pancreatitis, chronic fatigue syndrome, or vasculitis).
- Treatment patterns: Treatment started ~9 months after diagnosis. Managed primarily by rheumatology (70%). Most common first therapies were prednisone (66%), rituximab (17%), and azathioprine (11%).
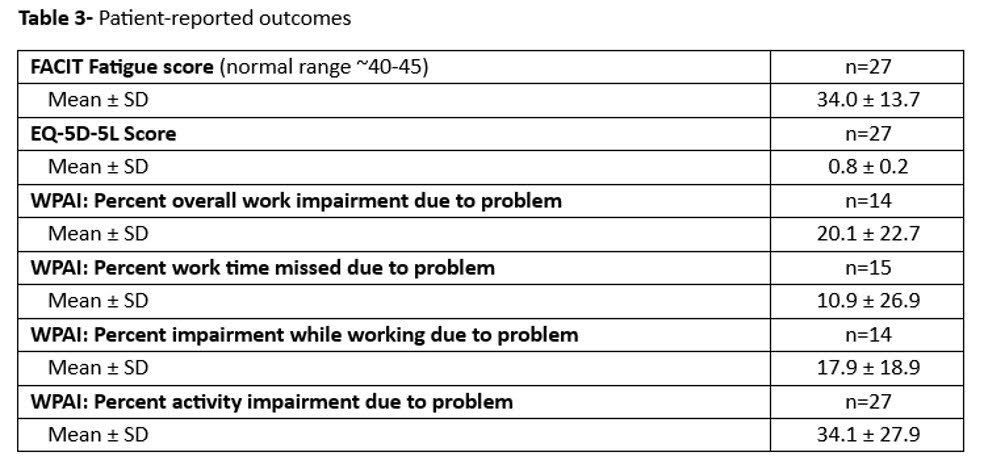
- Hospitalizations & impact: 14% were hospitalized in the prior year, mostly through the emergency room. Patient-reported outcomes showed notable impacts on fatigue, daily functioning, and quality of life.
Conclusions
This real-world survey highlights how challenging and time-consuming the diagnostic journey can be for people with IgG4-RD. Many patients face long delays, multiple tests, and frequent misdiagnoses before receiving proper care. Symptoms often affect quality of life, and treatment is highly variable. These findings underline the need for greater awareness, faster diagnosis, and more effective long-term management to improve daily functioning and overall health for patients living with IgG4-RD.
Key Data:
- 161 patients reported; 27 completed patient surveys.
- 11.5 months average time to diagnosis.
- 90% initially misdiagnosed.
- Most affected organs: pancreas (32%), parotid glands (22%), retroperitoneum (19%).
- Most common first symptoms: fatigue (42%), joint pain (23%), weight loss (22%).
- First-line treatments: prednisone (66%), rituximab (17%), azathioprine (11%).
- 14% hospitalized for IgG4-RD in prior year.
- Significant impact shown across fatigue, daily functioning, and work productivity.
Authors
Yasmin Hernandez-Barco (Massachusetts General Hospital; Harvard Medical School), Jenny Y. Park (Amgen Inc., Thousand Oaks, CA), Rajvi Wani (Amgen Canada Inc., Mississauga, ON), Andrea Meyers (Amgen Canada Inc., Thousand Oaks, CA), Matthew Charles Baker (Stanford University, Menlo Park, CA), Leonard Calabrese (Cleveland Clinic, Cleveland, OH), Kristina Patterson (Amgen Inc., Thousand Oaks, CA), Hannah Connolly (Adelphi Real World, United Kingdom), Shiva Lauretta Birija (Adelphi Real World, United Kingdom), Emma Culver (John Radcliffe Hospital; University of Oxford).
Read the published abstract in ACR Meeting Abstracts
IgG4-RD Education by AiArthritis
Go With Us! To EULAR 2025: What is IgG4-Related Disease -- and Why Are So Many Patients Misdiagnosed?
In this Go With Us! video from EULAR 2025, Health Education Manager Leila P.L. Valete breaks down key insights from a session on IgG4-related disease (IgG4-RD)—a rare immune condition that’s often confused with other autoimmune diseases like lupus, Sjögren’s, or rheumatoid arthritis.
This video covers:
- What IgG4-RD is and why it’s so tricky to diagnose
- What “SACQ” means (and why high lab numbers don’t always mean symptoms)
- How doctors use histology (tissue samples) to confirm diagnosis—and where that can go wrong
- A look at current and emerging treatments like Inebilizumab (Uplizna) and Ruznilomab
- Why understanding this disease is key for “mystery patients” who still don’t have answers
Thank you to Amgen for supporting our IgG4-RD content