AiA Episode 111 podcast FINAL
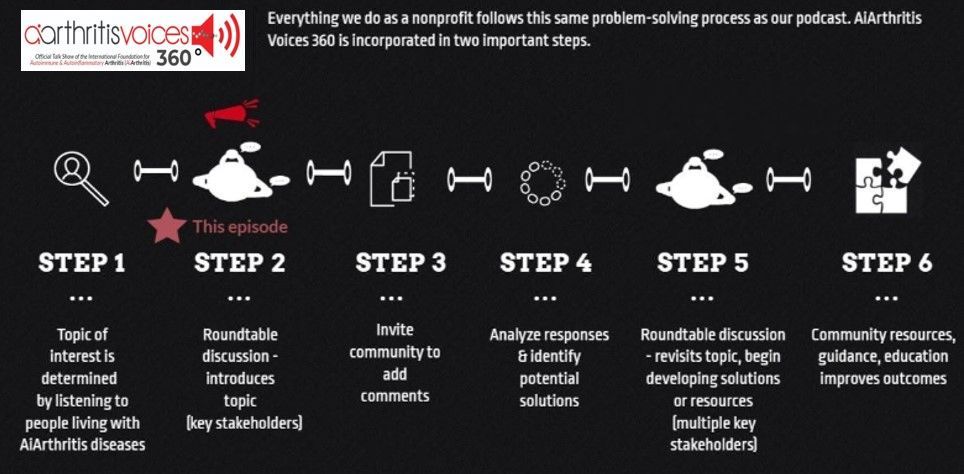
Intro: [00:00:00] Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table, where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient cohosts as they lead discussions in the patient community, as well as consult with stakeholders
worldwide.
To solve the problems that matter most, whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table.
Leila: Hello everybody and welcome to AiArthritis Voices 360, the official talk
show for the International Foundation for Autoimmune and Autoinflammatory
Arthritis, or AiArthritis for short. My name is Leila and I am your host Today. I am person living with Lupus and Sjogren's Disease, and I am the health education manager here at AiArthritis.
Today we have a very special episode for you. We are bringing you breaking research updates from the European Alliance of Associations of Rheumatology or Eular Congress in Barcelona, Spain that we just came back from two weeks ago. And you'll hear four separate updates from our in-person team, including me.
Our CEO and person living with non-radiographic axial spondyloarthritis.
Tiffany Westridge, Robertson Talk show, co-host, longtime volunteer, and go with this program Co-founder Deb Constein, living with rheumatoid arthritis and our patient advocate slash AiArthritis educational media assistant Eileen Davidson, also living with rheumatoid arthritis, and she's known online as Chronic Eileen.
In these updates, we will discuss different topics relevant to those living with aiarthritis diseases, including nutrition, cannabis use, and new innovative treatment options called CAR T-cell therapy, or just cell therapy in
general. So we hope that you enjoy these next few clips and I'll talk to you after.
Deb: Hey guys, it's Deb Constein tuning in from Eular Day one, and I am doing my debrief now. You're going to see me looking over here, my computer's over here with some slides for little triggers for me, and I wanted to let you know more about the session that I saw on the nutrition and microbiome. So there were three parts of it.
The first one was very basic and would be really hard to explain. The second one, there was some key terms that I wanted to just go through with you guys.
And the second section was called Targeted microbiome interventions and their impact on treatment response and prognosis examples beyond rheumatology.
So that's what that part was about and the one piece that really stuck out to me was it talked about microbiome interventions from global to targeted treatments and the global interventions that this is a new term to me. They said it's going towards precision nutrition. So again, creating things that are very specific to you as the patient.
I found that fascinating 'cause there's always been precision medicine that we always hear about things in this global interventions include whole diet, the gut, fermented foods, lifestyle, probiotics, things like that. And when we talk about targeted interventions, we're talking more about engineered probiotics as well as antibiotics and like mechanically engineered probiotics that are
made specifically towards you as well. So that was one thing, and it was talking about, so precision nutrition and cardiometabolic diseases, and I'll explain that in a second. And it was talking about the microbiome composition predicting biomarkers. And things like fasting and lipidemic and inflammatory indices, so all of your markers that you have in your blood.
I found that really interesting. The definition about cardiometabolic diseases are
a group of conditions linked to metabolic disorders and cardiovascular issues
including heart disease, stroke, diabetes, insulin resistance andnon
alcoholic fatty liver disease. So really interesting topic that covered a lot of
things.
But the third piece I think is really what we could dive in a little bit deeper. It was nutrition in the prevention and management of inflammatory rheumatic diseases. Speaker was outstanding and just covered so many different pieces.
First section, what do we know about nutrition being diet and supplements for prevention of our diseases, our inflammatory diseases like dietary patterns, dietary content, the vitamin D, Omega-3 fatty acids.
I know we've heard about those things before. This dives deeper and has some great resources related to that. This person was from the speaker, she had some cohorts, so there's a nurses health study cohort that included 121,700 women, age 30 to 55 in 1976. Then there was another cohort that was 116,761 women aged 25 to 40 in 1989.
So very detailed. Their nurses detailed diet reports and lots of questionnaires and things like that. So. They did find that RA and Lupus validated the cases that they had in chart reviews. So to prove the facts for a study, they actually did chart reviews to find the deep dive on who ended up getting rheumatoid arthritis and how many people got lupus.
So incredible information there. The second one that was really incredible was a cohort that they had of black women health study. 64,500 black women, aged 21 to 69, recruited nationwide, and it was. From 1995 to 2015,
and they had a lot of self-reported new cases that of lupus confirmed by the medical record review and by two rheumatologists, they found that the mean age of diagnosis was 43.
And there were 127 incident lupus diagnoses as well as, let's see, 31% of these lupus patients had nephritis at the presentation of the disease, meaning kidney disease. So good stuff. There was some different patterns of medicine that they looked at. They looked at the dietary quality scores and patterns examined in the nurses' health studies, and they found, no surprise. The Western diet, they had lots more instances of air, foods and
desserts, sweets, refined grains, processed meats, french fries, condiments,
things like that, and pizza that they were much more, they got diseases like RA
and Lupus much more, which again, no surprise. Let's see, what was another
one?
They looked at the lupus scores. There was no significant relationship with the risk of lupus and. They did notice that the black women cohort that I talked about, they did have a higher glycemic load, so they were a little bit
higher on the sugars in their diets and in their blood, in their labs that showed up.
So it caused an increased risk for lupus in general because of that. A term that I
hadn't heard before is ultra processed food. So if you think about like corn on the cob that is minimally processed. The processed is like a can of corn, but the ultra processed is like doritos, potato chips, things like that.
And definitely all of these things are associated with cancer, obesity, diabetes,
increased mortality, so not great news there. But again, a lot of people have a lot of these things that are significant in their lives. So what do we know about the effects of treatment of rheumatic diseases with diet and
supplements?
And this goes back to some of the things that we've heard before about the vitamin D and the the fatty acids. So. It talks first about how does inflammatory rheumatic disease develop and how does it spiral outta control? So it starts with a genetic disposition, typically then goes into the environmental triggers that are around us.
The innate immune system is activated. Then the adaptive immune system's activated. You have your immune complexes and you have clinical disease on set At that point, then. There's amplification of the disease in your body with irreversible tissue damage, and the sad part is this is cyclical, so it keeps happening over and over. So that's how our diseases spiral outta control. There were some studies, so one study or actually. A summary of 20 studies that talked about trials of Omega-3 fatty acids for ra. And all of these studies had strong evidence of beneficial
effect in RA being fatigue and disease activity, pain, all those big triggers.
So really interesting information. Now, there was a summary of. Nine studies of the trials of Omega-3 fatty acids and we're talking about the capsules. It can also be found in things like salmon and real fatty fishes. So fish, I guess that's the pearl. Sorry, it's after 11 o'clock here. And a little tired.
Sorry about that. But for the outcome for that for lupus showed six of the nine studies showed clinical or biomarker benefits. So there's things in our body that their lab work and things like that. Again, the fatigue, pain,
inflammation, all those things, it showed that there was a beneficial outcome. So gotta love that.
The summary of that session was healthy lifestyle and healthy diet. Obviously,
especially fiber and fish likely reduce the risk of severe autoimmune diseases and reduce the inflammation. I. The avoidance of those UPFs, which was the ultra processed foods. That's what we're talking about there. So avoidance of those things.
The super, super processed foods, long-term use of about. 2000 IU per day of Vitamin D. It does reduce the incidence of autoimmune disease by 22%. That's significant. There were varying dosages and the duration of vitamin
D that had been tested for treatment of lupus and ra, and there was no real strong consistent effects.
It definitely did have benefits on their pain scores. The DAS survey that you fill
out about how much it's causing effectiveness, the fish oil supplements are
likely to decrease risk of systemic inflammation driven the inflammatory
rheumatic disease and was proven to decrease RA disease activity. So the
tenderness of joints are pain, those type of things.
So it was an excellent session and I'm happy to answer any questions you might have after. You see the debrief come through that comes out tomorrow, I believe our day two, as we're learning more information and more information to report back to you. I'm talked in a little room in the kitchen here.
The other side is where everybody else is and they're getting all of their things organized as well. So great to see you guys here and tune in tomorrow.
Tiffany: Hi everyone, this is Tiffany and I am reporting from Eular 2025 in Barcelona, Spain, person living with non-radiographic axial spondyloarthritis, which is one reason that this session was of primary interest for me. People living with spondyloarthritis diseases like axial spondyloarthritis and psoriatic
arthritis often deal with something called enthesitis, and that is the area where the tendons ligaments connect to the bone and it becomes inflamed, and that is the pain we often feel even more than joint pain in our diseases.
And so we've been seeing enthesitis being studied more and more over the last couple of years. And this time it was talking a little bit more about different ways of tracking onset of enthesitis, what could cause enthesitis, and then going in that direction to see how to target treatments to match that pathway. One of the reasons for doing that too, that I think is worth noting is in these spondylitis
diseases, you know, we're all, we often go to the doctors and we're still talking about joints and enthesitis actually, when that is inflamed itself, the enthesitis, because it's right next to the synovial tissues and it's right next to the bone.
Inflammation of the enthesitis can actually lead to inflammation of the tissues. Synovial tissues lead to the joint damage, so in a roundabout way, joint damage can happen through cycling through enthesitis.
Equally, the enthesitis as it's inflamed can work its way into the bone. Okay. So in saying all of this, they started the presentation by talking about an onset that we know exists in many of our diseases, and that is gut inflammation.
And they were using that specifically as a comparison to think about these,
again, different treatment pathways, things that we should be looking at, where
inflammation starts, and then how the inflammation spreads. That was sort of
the big theme here. And so in gut inflammation, we know about 60% of patients
with psoriatic arthritis will have some kind of, what they call subclinical diagnosis of a gastrointestinal issue. And subclinical just simply means that it hasn't really developed enough to be one full diagnosis. And so in saying that, we know that the gut, it migrates outside of, you know, the system. And that's
the environmental trigger that starts our diseases.
And so then they also made a note that even though about 30%, they say about 30% of patients with psoriasis develop into psoriatic arthritis. People with psoriatic arthritis, whether it started with psoriasis or not, those with psoriatic arthritis of those 80% will experience psoriasis. So whether it just
started a psoriatic arthritis with the whole psoriasis onset, or with psoriasis first
that developed, it's about 80% total that will have the psoriasis.
And because of that, they felt if you observe the skin lesions, in particular in psoriasis and the genes and the cells, the T cells in particular that are responsible for chronic disease and live in the skin lesions, that following that path through the skin. The inflammation then crosses barriers and can affect inflammation of the enthesitis.
So the enthesitis being, you know, where the ligaments in the tendons are connecting the bone, and so this enthesitis then also once that is inflamed, so it's like this chain reaction that they were studying. Once the enthesitis is triggered, then the enthesitis could lead to. Synovial tissue inflammation, synovial tissue inflammation leans to joint issues, so joint
deterioration.
It also can lead to bone deterioration. And so when we see the bone deterioration, in these diseases. Then we've got this whole kind of, so there, the idea was if we can identify if the skin lesions are potentially a primary driver of
inflammation, so let's just move away from the gut bacteria for a minute and we look at for psoriasis and the skin lesions in particular.
If we can follow that chain of event, then possibly we could match people with
significant or treat to target like you might respond better to A TNF inhibitor or something, et cetera. So it was just a different way of thinking about research and I believe it had mentioned, and I am going to say I missed the first five minutes of the presentation, so I believe that they said also because they ended the conversation too by saying it would be important to continue studying the number of psoriasis, to psoriatic arthritis, things to watch.
And so would this be something if people are complaining about psoriasis plus this enthesitis. And being able to better diagnose enthesitis, could that then improve the diagnosis to psoriatic arthritis.
So that is the link. And so they talked a little bit too about differentiating enthesitis from mechanical injury or overuse. So similar to we hear about joint inflammation, where it could be from overuse. Excessive pressure on the joint, or it could be from disease. It's the exact same with enthesitis. So enthesitis that inflammation between the bone or the tendon ligaments.
That also can happen from overuse and injury. So just making it it, is it from that or is it from disease? If you can rule that out and say it's from disease plus you have this psoriasis, then in addition to the pathways of having the skin go through and infiltrate the inflammation to the enthesitis, and we could make, you know, study those patterns of the cells that connect the two, then we could
have a better treatment plan, but also could it be something for diagnosis.
So that was just something that I really found fascinating. You can see many other previous go with us where I talked specifically about enthesitis. It's been a very, very hot topic here at the conferences, which means it's something that's being studied more and more, which is exciting in spondyloarthritis.
Leila: Hello everybody and welcome to go with us to Eular 2025. My name is Leila and I am the health education manager here at AiArthritis, and I'm super excited to report back on the CAR T Cell Therapy. Session that I went to on day one, or it's not just CAR T cells, but cell therapy in general. They're changing
the language saying that there's other cells that they are able to do this therapy
for, and a lot of research going into these new types of therapies that are coming out, and there's lots of promising data showing that there can be long-term drug free remission.
This all started in the cancer space. This has been a really hot topic for autoimmune diseases and the rheumatic space in general. Being able to transfer this novel therapy into our space that came originally from cancer, and that's how a lot of drugs for air arthritis disease, it actually start is from cancer and being able to control cancer and then trying to therefore switch it over to the autoimmune side.
And so I have my notes on my phone so that I know what I'm talking about and making sure I don't miss anything. So I'm just gonna be looking at this to give me some of my notes. And so. I already mentioned that it all started in cancer.
And so now that these trials, and there's been lots of success in the cancer space, there has actually even been someone that they had shown a picture of that was a cancer patient who was in complete remission for over 10 years, and they even went to the point of seeing that it was cured.
And so right now the space that they are doing most of the testing in the autoimmune space is with lupus, systemic sclerosis, or scleroderma, as well as myositis and lupus and systemic sclerosis are both AiArthritis diseases, but myositis is not, it is closely related, but has to do more with the muscles than it has to do with joints.
And so this is a really interesting type of therapy and we've talked about it and
different go with us to conferences in, in 2024, but even in just a year, there's been so much new research that is here to present. And what is CAR T cell therapy or cell therapy in general? It is, I a treatment where they are able to take your cells and infuse you with engineered version of your own cells to basically reset your immune system and put it into a state that is no longer fighting itself.
And so now this is, it's been known to be a pretty invasive treatment because they have to really keep an eye on you because they're basically resetting your whole immune system. What we've seen is patients go in and get their B cells depleted, so they go through a round of a chemotherapy drug to get their B
cells depleted, and then they get their cells taken from their body. It's engineered and then put back into your own body and infused just once, and then they would keep you in the hospital for two weeks for observation just to make sure nothing goes wrong. So it's a very long process. And during that B
cell depletion phase, and when they're engineering your cells, you have to wait
for that and you're in a state where your immune system is very compromised, so you can't do much.
So it's about a six week process that can take a long time. But what's really cool now is that they're finding that they can create this therapy, not you don't have to do it from your own cells, that they can have donor cells that they are creating to infuse you with so that you don't have to wait so long to be able to give those re-engineered cells back into your body. And so that is one of the things that they talked about a lot yesterday. And so this is called allogenic or off the shelf CAR T cells, and it's manufactured from donor T cells and can be pre-prepared and stored. It's also potentially cheaper and faster to administer because you don't have to go through the personalized engineering easier to mass produce and it can be used off the shelf for multiple patients.
So this is a really big thing that they are seeing. When we were just at ACR in November, we got a whole presentation on how CAR T-cell therapy works.
And so this is amazing to see that they're already coming up with ways to make this more accessible to patients. Make it affordable. Make it so that insurances will be able to pay for it, because as it stands right now, way too expensive, only available in clinical trial form.
And just being able to see the progress of this over the past year has been amazing and. Like I said, it's a single infusion treatment and has potential for drug-free remission. There has been one patient that they also presented that was a lupus patient who has been in drug-free remission for four years already, and so they definitely won't get to the point just yet where they can say that it's a cure.
But long-term drug-free remission is an amazing endpoint and an amazing place
to be where it's almost even close to being a cure. But we are going to still continue to see what happens over the next few years for these patients that have gone the clinical trials and have gone through the CAR T-cell therapy.
And yeah, that's, it's really an amazing novel treatment to see how much science has evolved in the past years. And so there are some safety considerations when thinking about CAR T cell therapy, and there is something called cytokine release syndrome that can happen that if your body reacts negatively to the infused cells.
There also could be local inflammatory reactions like a rash or things like that, but usually can be easily taken care of and there also could be potential for short term corticosteroid use to calm down the inflammation in the body as the treatment is going on. But they all seem like pretty mild safety considerations when talking about this therapy.
The benefits of the therapy is that it can penetrate cold tissues. There's rapid B cell recuperation, so even though the B cells do get depleted to be able to reset the immune system, the B cells are able to recuperate and recover and become active and protective really fast afterwards. And yeah, it has the highest potential to reset the immune system just because you get the B-cell depletion
and the CAR T-cell infusion.
The hope is for your immune system to be reset and it, we have seen that happen, but there have been very few where it still helped but not have maybe done a full reset of the immune system, but it has significantly improved how many medications you have to take or how much. Day-to-day symptoms you may have.
So even if a full autoimmune res or immune system reset is not completed, there is still significant change and significant improvement to day-to-day life than there was before. The last thing that is really important for all of you all is that they're also looking to expand to other autoimmune conditions as soon as possible.
One of the ones that they mentioned is ITP or immuno thermo Cytopenia. It's actually a low platelet autoimmune disease where it causes low platelets, and that's actually something that I had when I was eight years old that. Is seen now to be a precursor to lupus, so that's really cool for me to see that, that there's
new therapies for that as well, and hopefully very soon it will move into other AiArthritis diseases.
I don't see why it wouldn't work for these other diseases. It's just really making sure, getting the mechanisms to see that it will work in those other disease states. Super excited over the next few years to see where this goes it currently, like I said, is with systemic sclerosis, lupus and myositis, but very soon they look to expand to the other autoimmune diseases and autoinflammatory diseases.
And last thing is like the limitations of this, it's very complex and very extensive, like I said before so it's not something that's easily accessible. It's not a guaranteed permanent cure, but there is potential for, it's like I said, to significantly improve your day-to-day life and and symptoms, and there's lots and lots of ongoing research to see how this is going to continue to help arthritis patients, the arthritis community, and all other patients that are experiencing different autoimmune diseases like theselike always so many amazing new research and new discoveries at these different conferences that we go to. And here at EULAR 2025. CAR T is a really big theme, as well as there's a lot of other new treatments on the horizon.
I just wanted to do a whole video talking about this specific session because it was so in depth and so interesting to be able to talk about CAR T-cell therapy. I also wanted to thank. Bristol Meyer Squibb for sponsoring our Go With Us program and allowing us to be able to talk about CAR T-cell therapy to all of
our patients and all of our community, and let them learn how this therapy can really improve the lives of patients, hopefully here in the next 10 years, if not sooner.
So. Thank you again to Bristol Myers Squibb for sponsoring our Go with Us program. And thank you all for listening and I look forward to reporting back to you on day two of EULAR 2025. Alrighty, bye-bye.
Eileen: Hello, Eileen Davidson here. And, uh, my last sunny day here in Barcelona, I've had a little bit of technical difficulties, so had to redo some of my debriefs for you.
So this one is on cannabis, and this session was a debate between two doctors, one from Israel and one from the us. And they're kind of assigned a topic. It's not necessarily something that they specialize in, but they are assigned a topic and they're supposed to look through all the evidence and display.
This is the no side, this is the yes side, basically. So there were two questions
that they, um, had to kind of debate on, and then those in the audience that were healthcare providers would vote on two questions. One was do they prescribe
cannabis to their patients? And do they think that cannabis should be legalized?
So the results are kind of interesting. In the beginning, 35.4 said that they do recommend cannabis. And 64.86 said no. And then about legalization it was 68.97 said yes, keep it legal. And 31.03 said no. And that was at the beginning before the debate. Those numbers changed. So some of the arguments that they
brought up were interesting.
The first professor he brought up that cannabis has been used in history for a
long time, and recently the legalization of cannabis has actually created a high prevalence of cannabis use disorders and early, early use amongst adolescents and adolescents using marijuana is actually not very good because it affects our frontal lobe or our brains.
So it actually, it contributes to lower iq. He showed some systemic reviews
showing there was no significant pain reduction when cannabis is added to
opioid treatment. But he didn't really show many other reviews where wasn't
necessarily a pain relief for other conditions. He highlighted that there are health risks when taking cannabis, but just like our medications, there's also health risks. So he says that there is a significant lack of pain reduction in patients using cannabis for chronic pain. I'm curious, do you agree with him there? And he also highlighted the potential negative effects of long-term
cannabis, including increased sensitivity and severity of pain.
He also provides an overview of the current legal status of cannabis. Ed denote that while federal law considered is it a substance, many states have legalized it for medical and recreational use. He also went over that many CBD products that you buy in the store actually still do contain too much high dose of
THC, and that's concerning for those people that don't want too much THC, so they don't include, you know, any of the components that make you feel high.
He said that the risks, so cannabis use during pregnancy include a high risk of preeclampsia and maternal anemia, and he shared data on how increased risk of neonatal complications in babies born to cannabis use mothers. And he emphasized the need for rigorous campaigns and increased taxes to reduce
cannabis use, similar to the approach taken with cigarettes and opioids.
Then you focused on what it does to the mental health. So this, he said that it can, it's a correlation between cannabis use and mental health issues, including bipolar disorder and schizophrenia. And he showed that there
was some data, a high conversion rate to schizophrenia and bipolar disorder among cannabis users.
Have you ever heard of this or have you ever met anybody who has experienced this? And you know, with high THC products, cannabis products, that there is a higher increase of psychosis. And also there has been an increase in ER visits and risk of dementia among young adults who use heavy amounts of cannabis.
He also highlighted there are some cardiovascular health, uh, risks, including
increased blood pressure and reduced left ventricle ejection fraction. He shared
data that high doses of cannabis can also increase the risk of myocardial infraction. And hypertension but hypertension is low, high blood pressure, so sorry, I'm repeating myself.
The professor highlights also the mortality risk of cardiovascular diseases among cannabis users, but there wasn't really much, you know significant data on this. He emphasizes also the need to understand the long-term effects on cannabis health. So you'll hear over and over again that there's just not enough
research or evidence behind cannabis, and I see that there is more and more call
for this.
He stated that there is potential risk of cancer in patients using cannabis. And mostly frequent and long-term users. And again, he said more research needs to be on this and understanding the importance of balancing the potential benefits of cannabis and its known health risks. So then it went to the physician from Israel, and his side was the Yes side.
So he showed some background how cannabis has been used for centuries, even
in China, where it's now illegal. And you know, you talked about the different ways that you can use cannabis. It doesn't have to just be smoking. It can include inhalation with a vape or indigestion With edibles, you can even wear patches or topicals.
And then he also showed that there has been data that has shown that there is
benefit effects of cannabis on inflammation and pain management. So it's a little
bit confusing because they both are saying the wrong thing and it's like, well.
Where's the data highest and how are they doing these studies?
So yeah, it's kind of interesting you said that there was a number of benefits in treating, using cannabis to treat diseases, autoimmune diseases, particularly
rheumatoid arthritis and fibromyalgia. There's not many drugs for fibromyalgia or scleroderma, and these are two drugs that those patients have reported relief from, you know, including pain reduction and improved quality of life. So that's important, especially if you know the improved quality of life
part and that, you know, the cannabinoids, which are the anti-inflammatory part of cannabis can actually reduce inflammation. And like the other professor, he also highlighted there is so much more need for research in this area.
He did go over the side effects, including that, you know, it can include memory loss, psychosis, and addiction. So it's a little bit more rare.
And data showed the risk of addiction is lower than that of substance, like alcohol and
opioids. You know, proper dosing and supervision is important when prescribing cannabis to patients.
And once again, highlighting that there needs to be more long-term studies on the effects of cannabis and health. So that was kind of their whole argument.
And at the end, remember I said these numbers before? If they were recommend
yes, was 35.14, no was 65.86. But then at the end, after arguments, the ones that said that they would be willing to prescribe it to their patients went up to 40%
and then.
Actually went down to, no, but then this is where it was a little surprising
because remember the legalization numbers? They were originally yes. Keep it
legalized, and that was 68.97% and the no was 31.3% and it actually
changed a bit more. And in a direction that I wasn't kind of expecting. So
legalized actually went down to 66.7% and then that was for yes, keep it legal,
but no.
Went from originally from 31.3 down to 33.3 33. So you see how there's lots of
threes in those numbers. It's kind of a tongue twister, and I'm tired after the last
day of the conference, so I thought it was kind of interesting how people
thought maybe it shouldn't be legalized because one of the doctors also
highlighted that there has been an increase in ER visits.
There has been an increase in motor vehicle accidents, some cases where there
has been cannabis psychosis that have resulted in someone's death. However, he
showed news headlines or like Daily Mail, UK Edmonton News and some, uh, another one. And they were, well, they were nice headlines that are
gonna be eye catching.
As a writer, I know you should never just go by an article's headline. There could be more information in those articles that may say something like, use our head previous history of, uh, psychosis or mental health problems. So you, you need to take that in consideration. And then one thing the first speaker did not bring up, but the second speaker brought up that really stood out to me.
And as a patient with a rheumatic disease who does use cannabis as a pain relief. He said, or this is with the Israel one. He said that all of our medications have side effects too, sometimes even worse than cannabis. So it really should be a shared decision making between the healthcare provider and the patient.
Obviously, you know, you're gonna increase their health literacy. They need to know the risks, they need to know how to take it safely and be monitored. And I agree with that part. So I was happy to see that, you know,
the, yes they went up, that more physicians would actually be willing to help prescribe it to patients, especially those with ibromyalgia, scleroderma, and even though it's a study that was highlighted about rheumatoid arthritis, so I'm curious.
Do you think cannabis should be prescribed by providers or do you use cannabis for your, uh, any pain relief? And, you know, it's not just pain relief, there's mental health relief, there's sleep relief, and there was high studies
showing that patients who had pain from rheumatoid arthritis had a significant
decrease in pain and increase in sleep quality.
So that's really important. If we get better sleep, of course we're gonna have less
pain and you know, less symptoms throughout the day. So I'm curious, drop
your thoughts in the comments because I would love to read them and let's keep this discussion going.
Leila: All right, and those were our breaking research updates.
I hope that you enjoyed them. You can go ahead and check out our, go with us
to EULAR 2025 playlist on YouTube to find more videos that we created on all
of the different sessions that we attended. Specifically we have disease specific
videos on Sjogren's psoriatic arthritis, Veis syndrome, IgG four related disease,
lupus, rheumatoid arthritis, and stills disease, as well as more general topics like
pain management and transition of care from pediatrics to adult.
And so please go ahead and take a look at that playlist on YouTube where all of
the videos will be public by the time this episode comes out. And if you have
any questions about this episode or topics that you wanna hear us bring to the
table, you can email us at podcast@aiarthritis.org and [00:44:00] we'll definitely take a look at your questions and suggestions.
And if you enjoyed these research updates, sign up to go with us to ACR 2025. That is going to be this October 24th to 29th, and you can sign up at
AiArthritis.org/conferences as well as. We talked about last episode signing up
for the Meteorology Patient Summit. That is going to be September 13th and
14th in person at Mercy University in Dobbs Ferry, New York.
Or you can sign up for the virtual option and the link will be in the description.
As well as July is Juvenile Arthritis Awareness Month. So tune into all of our
social media channels to learn more about what AiArthritis does to support
juvenile arthritis patients and their families. Specifically, we are gonna be
premiering a new tool to help improve communication with healthcare
providers and families, specifically for juvenile idiopathic arthritis.[00:45:00]
And all of the healthcare providers that children and families may be seeing and
just helping to make sure that everybody's on the same page and understands
each other's goals and are able to have productive conversations. So we are
super excited to let you all get a glimpse at that new tool. And at AiArthritis, we
don't just represent the patient voice.
We are the patient voice. And with your support, we can amplify it even further.
If you found value in this talk show, please consider making a donation to help
us continue producing impactful conversations, bringing stakeholders to the
table to discuss patient identified issues and patient infused solutions.
You can visit AiArthritis.org/donate to help us make a difference together.
Thank you again for tuning into this episode of AiArthritis Voices 360. You can
find AiArthritis on all major social media platforms at IF AiArthritis, and that's
a wrap. We'll see you here next month. On [00:46:00] the next episode of
AiArthritis Voices 360.
Thank you,
Intro: AiArthritis Voices 360 is produced by the International Foundation.
From autoimmune and autoinflammatory arthritis, find us on the
web@www.AiArthritis.org. Also, be sure to subscribe to this podcast and stay
up to date on all the latest AiArthritis news and events.