AiA EP 11
===
[00:00:00] Hello and welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and Autoinflammatory Arthritis, or AiArthritis for short. My name is Leila and I am your host. Today I'm a person living with Lupus and Sjogren's Disease, and I am the health education manager here at AiArthritis.
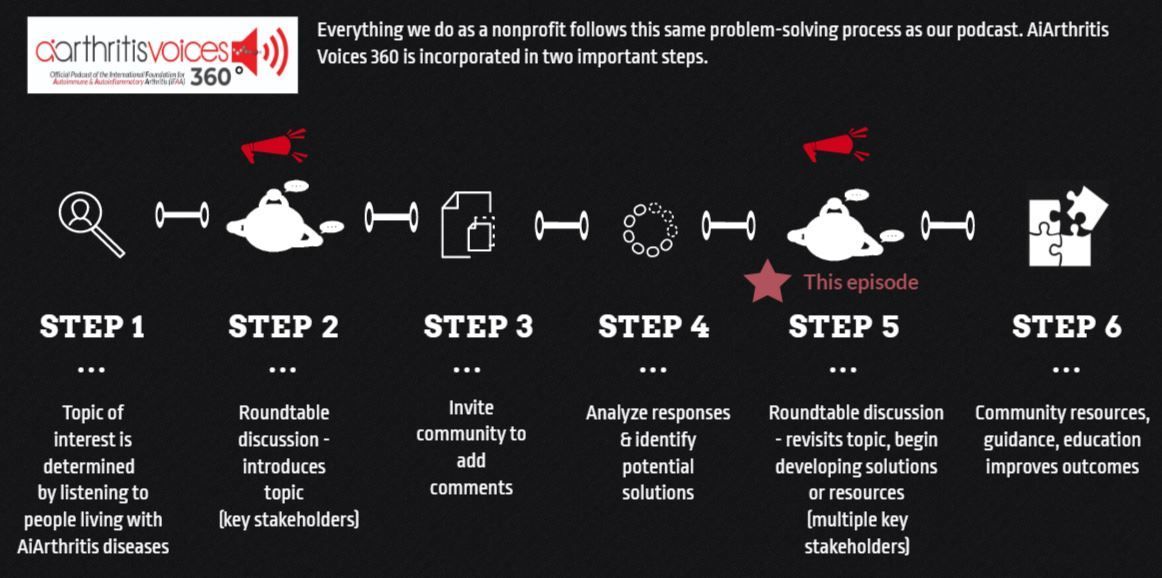
This episode is a step five episode, meaning we are bringing a topic back on the table. Today we will be discussing reproductive health, family planning, and pregnancy. The last episode we did on this topic was published in January, 2024, and we have several, several previous episodes under this topic as well that you can find if you search for this episode at www.AiArthritis.org/talk show. If you click on the most recent episode, you should also be able to see the links to all the [00:01:00] previous episodes under this topic as well. And so since the last time we published an episode about reproductive health and family planning, we have had one new episode of Go With Us.
And this is from EULAR 2024. So not this most recent EULAR, but EULAR last year. And I wanted to go over some of the important takeaway points from that specific video. And just as a reminder, when we are talking about these takeaway points, remember that the audience for. These conferences and for these presentations are rheumatologists.
So these are the recommendations for rheumatologists on what they should do with their patients when it comes to family planning. So the first thing is early and regular family planning counseling should be offered to all patients. Men and women emphasize that it should be brought up, up proactively.
So that's one thing that's super important, is that rheumatologists are talking [00:02:00] to their patients about family planning. And even if it's just a brief, you know, sentence or two conversation during a visit once a year or once every, you know, once every six months, but just, you know, bringing up the topic.
Are you still on birth control? How are you doing on that birth control? Is there any chance that you are plan looking to family plan in the next. Few years. And same thing with men asking if they're planning on family planning at any time in the near future. Because then, you know, treatment plan can also change depending on those questions.
And it's really important, like it says here to start early when a accounting for these changes that need to happen in treatment plan. And the next thing is emphasizing treat to target and aiming for remission or low disease activity before, during, and after pregnancy. So. Looking for that low disease activity or even remission is really important when it [00:03:00] comes to pregnancy.
There it's recommended that you are at least at low disease activity for six months before conceiving. So that's why knowing when you're planning to conceive and having this plan in place is so important. Again, because, unexpected or unannounced pregnancies can cause flare, can also cause you know, more issues with your condition.
Okay, next topic says, risk balance, weighing medication risks to fetus against risks of controlled maternal disease. This is nuanced and individualized. And this is actually something that was brought up at ULR 2025 as well, is this idea of, you know, really having to decide what is important at that time to that patient and also to their provider.
Having that shared decision making on outweighing the risk of what may happen being on this medication, what might happen to the fetus against what might [00:04:00] happen if. The mother's disease is uncontrolled, so that is very important because like it says here, it's very individualized. Each provider and each patient can have a different idea of what is important to them.
So it's really, really needed to have those conversations to know. What is going to be important, and I think the biggest thing is that, you know, reducing the risk of flare and reducing the amount of pain that the mother may be in during pregnancy. It is very important, but it really is up to that mother and that individual to decide what's important for them as well.
Another topic of breastfeeding. Don't discourage breastfeeding while using compatible meds. So again, this is talking to the rheumatologist you know, discussing transfer and immune impact considerations for the baby. So this is basically [00:05:00] saying, you know, if the mother is on if the mother is on compatible meds for pregnancy, then.
It is encouraged for them to still breastfeed and. Also if there is, if the mother is breastfeed, breastfeeding they may have questions about if the medication will transfer to the baby or if the medications may have some kind of impact on the baby's immune system. And so usually the medications that are safe for breastfeeding means that the medication does not transfer into the into the milk.
But, you know, sometimes there may be different situations that are happening. So each. Individual medication is a different circumstance, so having to talk to your own provider is, is super important to make these decisions. They mention here shared decision making across rheumatology and OB or maternal fetal medicine.
So it's talking about making sure that parts [00:06:00] of the party are helping to make these decisions when it comes to the specialist OB or the maternal fetal medicine doctor, as well as the rheumatologist. Making sure that a high risk OB is involved is usually what is required when it comes to people with R diseases.
Getting pregnant. So that is super important to make sure that you have a cohesive team that's put together so that they can communicate with you and also with the other doctors to come up with a universal plan that everybody agrees with. Next medication notes, of course. Making sure to discontinue cyclophosphamide for both men and women because it is very critical and, and it is also very critical for men preconception to make sure to stop this.
Discontinuing methotrexate and mycophenolate before pregnancy is also very important because those are not pregnancy safe and with JAK [00:07:00] inhibitors. There's a lot of data that is still limited, so make sure to, you know, err on the side of caution when it comes to JAK inhibitors specifically. And those are the points that we talked about in that go with us Video from last year's eular.
All still very relevant and like I said, with EULAR 20 20 25 this year. They specifically, emphasized and changed some of the guidelines to some medications to have this specific sentence that says, you know used to treat maternal disease. So basically making the decision on whether it's important enough for the me for the mother to have this medication in order to control their disease.
You know, versus the effects of what may happen to the fetus when it comes to these medications. So that is it's definitely an ongoing topic and it's really hard to have studies on these medications in pregnant [00:08:00] women because of the ethics and, you know, having volunteers for these studies would be very hard because you know, you, you know, maybe putting your, your baby at risk if, you know, participating in some kind of trial. So that can be it's really hard because there's less data, but it's also understandable because there's not a lot of people participating in these studies. Overall. And the next the next topic that I wanted to talk about is my own family planning update.
I talked a little bit about. What was happening in my family planning before changing some of my medications as well as having my bariatric surgery to make sure that I was in a healthier body, to be able to try to conceive. And so it's. About a year after making that update video my husband and I moved back home to where our family lives, and that's when we decided that it would be time for us to go ahead and start [00:09:00] trying trying to conceive.
And in March of this year of 2025, I removed my Nexplanon birth control and by. The end of April of this year in 2025. We had conceived and found out in about, in early June that we were pregnant. I actually found out the week that we left for Eular. So that was a very interesting situation to be in especially knowing that I was pregnant and coming in, hearing all those updates specifically on my own medications. It was very, very interesting to hear about and talk about. And yeah, it's been a, a really cool. It's been a really crazy first three months. You know, trying to navigate through all of the different doctor's appointments all the symptoms and all of the decisions that have, have had to be made.
So as of today, I am three months pregnant and we're looking to poss well, the due date is February 3rd. [00:10:00] And I'll talk a little bit about a lot of the decisions that, have started to, we've, we've had to start making decisions and the first one was, making sure to try and transfer out to a maternal fetal medicine doctor or a high risk ob.
And I had known what hospital I wanted to go to and, you know, which doctor I wanted to try to make sure that I could go to. So, luckily I had started that process before I found out that I was pregnant. So I had already started transferring over my doctors to this system. And once I found out that I was pregnant, I was able to go ahead and start making appointments with the high risk ob and so.
They are booked out very far in advance, as you can imagine. It's a very high demand for these types of appointments. And so I finally had my first appointment with them last week, and that was amazing to be able to go [00:11:00] in and speak with the nurse practitioner that was there. I had a video visit with the actual maternal fetal medicine doctor.
At the end of June, so about a month ago, and we went over a lot of different things during that. During that first interaction, she was getting, you know, history on my medication, on my disease and all of that, as well as what I'm doing right now with all of my medication. We adjusted some of the. Blood pressure medication that I was on.
I also was recommended to go see a nephrologist just in case there is any chance of my lupus nephritis or my kidney issues with my lupus flaring up again during this pregnancy. So as you can imagine, I am seeing maternal fetal medicine doctor that is almost every month, and that's virtual or in person.
Additionally to the maternal fetal medicine doctor, I have an OB GYN nurse practitioner that I [00:12:00] go to see for my regular OB appointments. I have a nephrologist that I'm seeing every two months, but getting labs every month just to make sure that there's no chance of my kidneys starting to act up. Or if there is, we.
You know, kind of intervene as soon as possible. And of course, seeing my rheumatologist. So I have not seen my rheumatologist yet during this pregnancy. I actually am going to have an appointment with her tomorrow, so that'll be very interesting. I think one of the biggest decisions that. I felt like I already had an, an answer to what the question is going to be about my specific medication or my biologic that I'm on, which is benlysta or Belimumab.
And I had been collecting a lot of information and data over the past three years as I was preparing for for trying to conceive, and I had gotten a consensus from several different rheumatologists that Benlysta seems to be. Safe [00:13:00] throughout the whole pregnancy. But the only caveat is if the if the molecule is transferring through the placenta to the baby the baby's immune system develops in the third trimester.
And so if the molecule. Going to the baby, it may cause the baby to have a weakened immune system or depleted, or a lower amount of B cells when it's born. And in that regard, there may be some vaccines that may need to be postponed or a few extra appointments just to make sure that the immune system you know, is, you know.
Increasing and, you know, kind of fixing itself after the baby is born. And so that was my idea before, was to go through the second trimester and then make a decision during the third trimester to see. What would be the best option And as I'm going through now and as, as I've seen the updates from EULAR 2025, I am leaning a [00:14:00] lot more towards continuing my benlysta through the third trimester.
And so that is still to be finally determined probably in the next two months. But so far so good with all of the other medication changes I had changed over from Mycophenolate to Azathioprine about a year ago, and I'm making sure, actually, sorry, I was off of my mycophenolate after my bariatric surgery and added azathioprine last July in order to have some kind of line of defense for my kidneys because I was not on any other kidney medication or kidney prevention medication besides my benlysta. So just because there's a higher chance of lupus nephritis flaring in pregnancy. Just because in regular pregnancy your kidneys can, you know, get a little damage from the overwork with the pregnancy and protein can leak through your [00:15:00] urine. So that's also what happens with lupus nephritis and they, that's why there is a higher risk of lupus nephritis possibly flaring up during, during pregnancy.
So making sure that I was on medication to kind of help with that was really important. As well as just making sure that I was taking prenatal vitamins since my birth control was taken out so that at any time if I did become pregnant, that the baby would already have the nutrients that was needed by having the prenatal at that time.
So I did start the prenatal you know, a week or two after I took out the birth control. And thank goodness I did because about a month later, that's when I ended up being pregnant. So that is super important because the first four weeks of development is, is important when it comes to the baby and their, their neural tubes or other types of structures that are forming during that time. Let's see, what else did I want to [00:16:00] talk about when it comes to this? So I did have that decision with the Benlysta come up again with this rheumatologist in their office. And as I said before, it happened to be that, I was having and making all these appointments after I came back from Eular.
And so I had known that the, the changes to the guideline happened, but my rheumatologist office did not know yet because it was just a week prior that it said now that Benlysta is approved to treat the underlying condition of the mother. And so originally my rheumatologist recommended that I stop my benlysta.
Right away and I had to kind of push back and let them know about. The guideline change in that. I've had conversations with several rheumatologists before and had already made the decision that I was gonna stay on Benlysta. And that was something that I'm, I was super adamant about and was not gonna let this rheumatologist [00:17:00] tell me otherwise.
And so it ended up working really. Working out really well because the maternal fetal medicine doctor actually agreed with me. And so we decided to keep going forward with the medication. And the other thing that I learned is that with Sjogren's disease, the SSA and SSB antibodies are, make you pre predisposed to fetal heart growth block, which basically means that there may be some issues with the, with the baby's heart developing or, or not becoming big enough during the pregnancy. And so because of that, I am. Going to be after week 30 would need to keep checking in with a fetal cardiologist, and they're gonna do fetal echocardiograms to check on the baby's heart and how it's growing and if anything needs to be done, if the baby's heart isn't growing at the right rate.
[00:18:00]
So there's that additional monitoring that needs to happen. I already had mentioned that I'm gonna have labs done every month. As well as just making sure to monitor for flares and high blood pressure as well. And, at the end, towards the end of the pregnancy as well. I believe after week 34, I will have to go to the office and meet with a nurse twice a week to do a non-stress test which is also to check on the baby's growth and to just make sure there is no growth restriction.
So that will start happening in week 34 as well, where I have to go to the nurse twice a week to go and get that done. And they said that that can last anywhere from an hour to an hour and a half. So as you can see, there is a lot of you know, appointments going on, labs imaging all of these different appointments that are very important to make sure that both the mom and the baby are safe.
And it's something that I did anticipate [00:19:00] for, I did not know just how intensive it would be but with the the hospital that I'm with, they do make everything very seamless and I'm very thankful for that because I can only imagine how difficult it could be to coordinate all of these tests and all of these results if you know, you're going to different doctors that didn't have the same system and all of these types of things.
So I'm just very lucky that everything is in one central place and the hospital that we're going to is, is quite close to our house within a 20 minute drive, so that's nice as well. And it also helps that I work from home. I, I, you know, it, it's very tough to be able to schedule all of these appointments and be able to go to them while also still working a job.
And so that's something also to consider while planning for pregnancy is knowing that there will be a few days where you may have to take a half day or you may have to take a day off to attend these appointments. With me. It's also, like I said, their [00:20:00] schedule is totally packed up, so whatever appointment I get, I kind of have to stick with because there's not many options.
So it can be really tough when it comes to scheduling. Last thing that I wanted to talk about is mental health when it comes to pregnancy. With lupus specifically, anxiety and depression are direct symptoms of lupus and with all of our diseases, anxiety and depression are very common and very high likelihood of comorbidity and, you know, this type of increase in medical care and attention that needs to be paid to you know, to this pregnancy can cause a lot of stress. One of my biggest. Goals during this pregnancy though is to reduce stress, and so I have been doing my best to try to clear my mind whether that be watching Netflix and listening to music, going on walks, hanging out with my husband and my dog.
Just making sure to try and be as free as [00:21:00] possible. And my husband has been, you know, such a great partner when it came to this, when it's come to this pregnancy, and has really done his best to help decrease my stress as well. And I think that's really important when it comes to, to, you know, planning a pregnancy when you have these diseases is you know, having someone there that can help you reduce your stress help take over some of the things that may need to be done in day-to-day life
because for me, the first trimester was very, very tough. When it came to morning sickness, fatigue, and, you know, kind of just attention that I had. It was, it was really tough to be able to juggle everything when I was so tired. You can imagine with our diseases, we are already so fatigued and with pregnancy this first trimester, in the very beginning, it felt like it was three times the amount of fatigue that I would've had with, you know, just my lupus symptoms.
So everybody's first trimester symptoms are different. Some people have morning stiffness, some people don't. [00:22:00] A lot of people do feel fatigue and get tired, but some people don't. And so it really just depends on each individual, what different symptoms you may have. But educating yourself and knowing what symptoms could happen could be very helpful so that, you know what you can do to kind of combat them.
And so there's there's lots of remedies out there for morning sickness. There's lots of, you know, ideas of what to do for all of the different symptoms. So knowing that while you're trying to conceive and doing that research, you know, beforehand is, is really important to kind of get your head on straight.
And I also am on medication for anxiety and depression and that was also another part of the care plan was deciding whether or not to stay on that medication. And it was kind of the same conversation. It was basically, you know, if you if you believe that this medication is helping you and was helping you before you got pregnant and will [00:23:00] help prevent anxiety and depression from flaring so much in the pregnancy, then it's more likely better for you to stay on the medication than to get off of it. There's, you know, minimal, there's minimal damage shown when on this medication when it comes to fetus and knowing knowing that it, it made it easier to kind of make that decision.
But of course, again, every medication is different. So having those conversations are, are super important in the beginning stages of pregnancy. And I just wanted to kind of wrap this up by giving some, you know. Things for next steps for you all when you are going through this with your, with your doctors, when you're at your next visit and you know, if you're planning on conceiving or trying to you know, become pregnant.
Start with the conversations of what will treat a target look like during pregnancy. What would, what kind of care plan would you have? If I were to get pregnant [00:24:00] right now, which of my medications are compatible for conception, pregnancy, and breastfeeding, and which aren't? Do you think that I would need a maternal fetal medicine doctor?
And how would you coordinate with them? If we stop this specific drug that I'm on, what's the risk of flare pain that may happen? Or what's the risk of, of my pain being higher? Those are some good questions to kind of start the conversation and ask your rheumatologist next time you see them, if this is something that is you know, top of mind or something that may be priority to you in the next two, three years.
Next, just remember that conception can take a long time. It's, it's average that it takes a healthy couple one year to conceive and conception can take longer. With our diseases. So discussing timing is super important. And even artificial reproductive technology options like IUI and IVF can be really important.
Again, this is why having these [00:25:00] reproductive health conversations often and early is important because what if a patient does wanna have kids but doesn't plan on having kids until they're 35 or 40? You know, then maybe. Egg freezing options may be, may be presented or other kinds of ways to kind of help with that family planning process.
Also one of the things that is super important is knowing if you have antiphospholipid antibodies, because that can be, you know, can change your whole trajectory of a pregnancy. That's been asked to me several times if I, I have asked antiphospholipid syndrome or if I have any of the antibodies because that is really important to know for pregnancy.
Lastly, again, if you're not trying to conceive right now revisiting birth control options like the IUD implant or mini pill because estrogen is. It, it can be risky to have estrogen only choices of [00:26:00] birth control. So discussing the other options like IUD and implant and mini pills may be a really good idea to talk with your rheumatologist and with an OB GYN or your primary care doctor.
Alrighty. Well, that was a lot of information and I'm super excited to be able to let you all know that I am pregnant and hopefully carrying out this pregnancy throughout the the month of January or around there and looking to, yeah, I'll give you some updates along the way. I will probably do updates not in a full episode format but probably in a 360 that you all can see still on YouTube and, still on all our website and all of the different platforms. And so if you are interested in more information about reproductive health, you can go to our reproductive health playlist on YouTube. That'll be linked below. Also if you're looking for information on pregnancy safe medications or anything else having to do with [00:27:00] pregnancy and different medications, you can go to mother to baby.org.
I also am enrolled in one of their. Pregnancy studies when it comes to my medication benlysta. So that is super important to kind of be able to give information about pregnancy safe medications. And so they create a lot of resources about that. So check that out on their website. And if you have any comments.
Questions or topic suggestions? You can email us at podcast@aiarthritis.org and today, August 3rd when this episode is coming out, AiArthritis is having an in-person event in St. Louis. Missouri called the Race Athon. This event is to share with the community what we do and provide them with access to our resources while also raising awareness for our diseases.
We're doing this in a fun, interactive way by inviting the public to race RC cars that represent our projects and programs, and we hope to bring this event to different [00:28:00] locations soon. So stay tuned for that and stay tuned on social media to learn more about how the event went, and see some pictures and videos.
And here at AiArthritis, we don't just represent the patient voice. We are the patient voice. And with your support, we can amplify it even further. If you've found value in this talk show, consider making a donation to help us continue producing impactful conversations, bringing all stakeholders to the table to discuss patient identified issues and patient infused solutions.
Visit arthritis.org to donate and help us make a difference together. Thank you again for tuning into this episode of AiArthritis Voices 360. You can find AiArthritis on all major social media platforms at IF AiArthritis, and that's a wrap. We'll see you here next month. On the next episode of AiArthritis Voices 360.