Familial Mediterranean Fever (FMF): A Comprehensive Overview
How Common is Familial Mediterranean Fever (FMF)?
Familial Mediterranean Fever (FMF) is most prevalent among individuals of Turkish, Armenian, Middle Eastern, North African Jewish, and Arab descent. In some places like Armenia, about 1 in 5 people carry a mutation related to FMF. Here are some key points about its prevalence:
- Turkey: FMF is highly prevalent, with estimates ranging from 1 in 150 to 1 in 10,000 people, depending on the region.
- Armenia: The prevalence is about 1 in 500 people, with a carrier rate of 1 in 7.
- Israel: Among non-Ashkenazi Jews, the prevalence ranges from 1 in 500 to 1 in 1,000, while among Ashkenazi Jews, it is much lower at 1 in 73,000.
- Other Regions: FMF has also been reported in Greece, Italy, Japan, and China, but at lower prevalence rates.
- The carrier rates for MEFV gene mutations vary among different ethnic groups, with 1 in 5 among Iraqi Jews, 1 in 3.5 among Moroccan Jews, and 1 in 4.3 among Muslim Arabs
Causes and Genetic Basis of Familial Mediterranean Fever
FMF is caused by mutations in the MEFV gene, which encodes a protein called pyrin. Pyrin plays a crucial role in regulating inflammation in the body. When mutations occur in the MEFV gene, it disrupts the function of pyrin, leading to uncontrolled inflammation. The disorder follows an autosomal recessive inheritance pattern, meaning that an individual must inherit two copies of the mutated gene (one from each parent) to develop FMF.
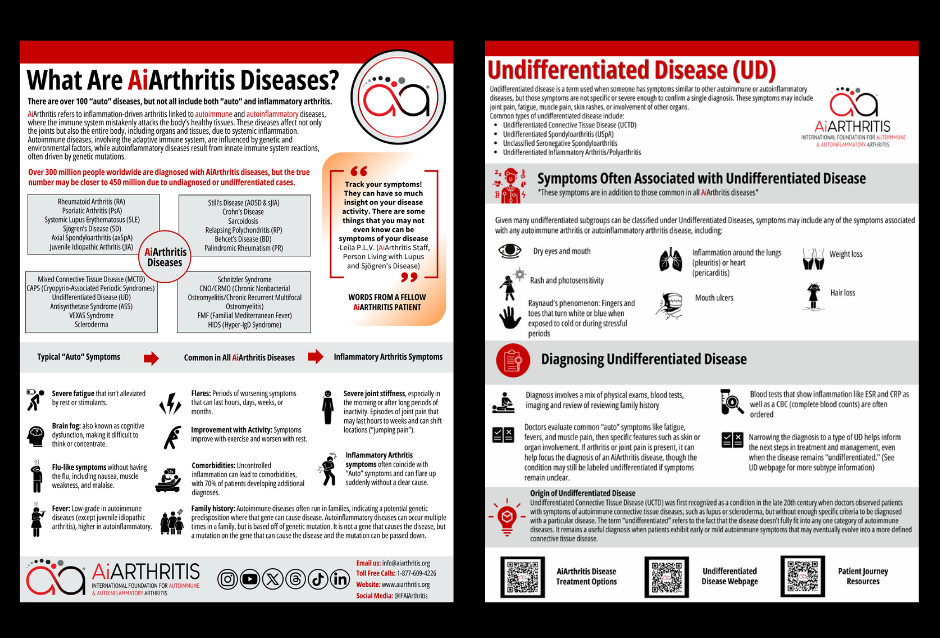
AiArthritis Disease Symptoms
AiArthritis diseases share common features such as flares, where symptoms worsen for hours to months, and improvements with physical activity, while rest can make symptoms worse. Genetic predisposition or mutations can lead to these conditions running in families, and uncontrolled inflammation often results in comorbidities, affecting 70% of patients.
Key symptoms include:
- Severe fatigue that persists despite rest or stimulants
- Brain fog, making concentration difficult
- Flu-like sensations like nausea and muscle weakness
- Low-grade fevers (higher in autoinflammatory diseases)
- Joint stiffness, especially in the morning or after long periods of inactivity
- Sudden, shifting joint pain that starts and stops abruptly
Symptoms and Attacks of Familial Mediterranean Fever (FMF)
Symptoms of FMF typically begin during childhood and manifest as sudden episodes or "attacks" that last from 1 to 3 days. These attacks can vary in intensity and frequency. Common symptoms include:
- Fever: High fever is a hallmark of FMF attacks.
- Abdominal Pain: Severe abdominal pain resembling peritonitis (inflammation of the abdominal lining).
- Chest Pain: Pain in the chest, often due to inflammation of the pleura (pleuritis) or pericardium (pericarditis).
- Joint Pain: Painful, swollen joints, usually in the knees, ankles, and hips.
- Rash: A red rash on the legs, particularly below the knees.
- Muscle Aches: Generalized muscle aches.
- Scrotal Pain: In males, inflammation of the tunica vaginalis can cause a swollen, tender scrotum.
Learn More About Familial Mediterranean Fever (FMF)
Quality of Life with FMF
One of the most serious complications of FMF is amyloidosis, a condition where abnormal proteins (amyloid) accumulate in organs, particularly the kidneys, leading to organ dysfunction. Early diagnosis and treatment are crucial to prevent this complication.
Familial Mediterranean Fever (FMF) can significantly impact the quality of life (QoL) of affected individuals.
Here are some key ways it affects daily life:
- Physical Impact: Recurrent fever episodes and chronic pain can lead to physical limitations, affecting mobility and the ability to perform daily activities. This can result in missed work or school days and reduced overall physical functioning.
- Psychological Impact: The unpredictability of FMF attacks can cause anxiety and stress. Chronic pain and frequent hospital visits can also lead to depression and emotional distress.
- Social and Recreational Impact: FMF can interfere with social interactions and recreational activities. The need for frequent medical care and the fear of sudden attacks can make it difficult for individuals to participate in social events and maintain relationships.
- Sleep Disturbances: Pain and discomfort during attacks can disrupt sleep patterns, leading to fatigue and decreased energy levels. Poor sleep quality can further exacerbate the physical and psychological burden of the disease.
- Impact on Work and Education: The physical and emotional toll of FMF can affect performance at work or school. Frequent absences and reduced productivity can hinder career advancement and educational progress.
- Healthcare Burden: Managing FMF requires regular medical appointments, medication, and sometimes hospitalizations, which can be financially and logistically challenging.
Despite these challenges, effective management and treatment can help improve the quality of life for individuals with FMF. Regular follow-up with healthcare providers, adherence to treatment plans, and psychological support are crucial in mitigating the impact of the disease.
Discover More Of Our Resources
Diagnosing Familial Mediterranean Fever
There’s no single test that can confirm a Familial Mediterranean Fever (FMF) diagnosis, so rheumatologists rely on a combination of physical exams, genetic testing for mutations in the MEFV gene, and family history of autoimmune or autoinflammatory diseases, as well as ethnicity, since FMF is more common in certain populations. While genetic testing for the MEFV mutation is important, the absence of mutations does not completely rule out FMF. In some cases, doctors may start patients on Colchicine to see if symptoms improve, as a positive response can strongly suggest an FMF diagnosis.
The Tel-Hashomer criteria are also used to aid in diagnosis. Patients must meet more than one major criteria or more than two minor criteria:
Major criteria:
- Attacks of generalized peritonitis
- Pleuritis (unilateral) or pericarditis
- Monoarticular arthritis of the hip, knee, or ankle
- Fever as the only symptom
- Incomplete abdominal attacks
Minor criteria:
- Incomplete attacks involving joints, chest, or both
- Leg pain with exertion
- Favorable response to Colchicine treatment
- Typical attacks are recurrent (at least three episodes of the same type), febrile (rectal temperature ≥ 38° C), and short in duration (12 hours to 3 days)
Complete attacks are painful, recurrent, and usually follow a predictable pattern, but they may differ in some features, such as lower temperatures (< 38° C), variation in attack length (6 hours to 1 week), or atypical symptoms like localized abdominal attacks or arthritis in joints other than the hip, knee, or ankle.
Though there are no specific ACR or EULAR guidelines for FMF, these organizations emphasize comprehensive evaluation, including genetic testing and clinical response to treatments like Colchicine, to ensure an accurate diagnosis and proper management of the disease.
Treatment and Management of Familial Mediterranean Fever
While there is no cure for FMF, treatment focuses on managing symptoms and preventing complications. The primary medication used is colchicine, which helps reduce inflammation and prevent attacks. For those who do not respond to colchicine, other medications that block interleukin-1, such as canakinumab, rilonacept, and anakinra, may be prescribed. Regular monitoring and follow-up with a healthcare provider are essential to manage the condition effectively.
Familial Mediterranean Fever is a complex genetic disorder that requires careful management and treatment to prevent recurrent attacks and complications. Understanding the genetic basis, recognizing the symptoms, and adhering to a treatment plan can significantly improve the quality of life for individuals with FMF.
Related Blog Posts
November 30, 2024
Highlighting the 2024 American College of Rheumatology abstracts on Familial Mediterranean Fever