Understanding Mixed Connective Tissue Disease (MCTD)
AiArthritis Disease Symptoms
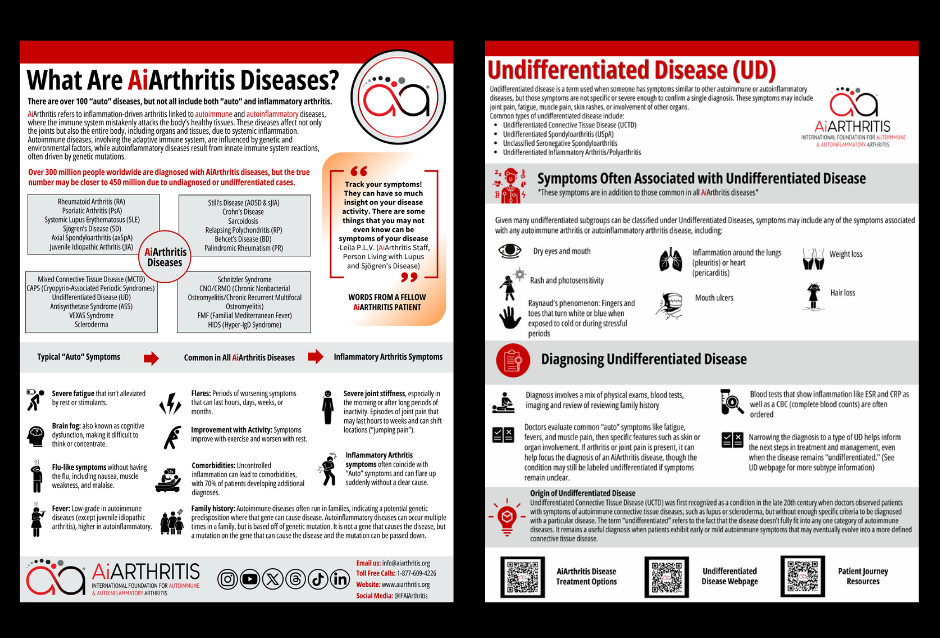
AiArthritis diseases share common features such as flares, where symptoms worsen for hours to months, and improvements with physical activity, while rest can make symptoms worse. Genetic predisposition or mutations can lead to these conditions running in families, and uncontrolled inflammation often results in comorbidities, affecting 70% of patients.
Key symptoms include:
- Severe fatigue that persists despite rest or stimulants
- Brain fog, making concentration difficult
- Flu-like sensations like nausea and muscle weakness
- Low-grade fevers (higher in autoinflammatory diseases)
- Joint stiffness, especially in the morning or after long periods of inactivity
- Sudden, shifting joint pain that starts and stops abruptly
Symptoms Specific To Mixed Connective Tissue Disease
- Raynaud’s Phenomenon
- Difficulty swallowing
- Hair loss
- Lung involvement (shortness of breath)
- Lupus-like skin inflammation in areas exposed to the sun
- Associated with Lupus, Scleroderma and Sjögren’s disease
MCTD is marked by a range of symptoms that may vary widely among individuals. Common indicators include Raynaud's phenomenon, where fingers and toes turn white or blue in response to cold or stress, swollen fingers, muscle and joint pain, and skin rashes. The joint symptoms in MCTD can mimic those of rheumatoid arthritis, including pain, swelling, and stiffness. However, unlike rheumatoid arthritis, MCTD may also present with features of other connective tissue diseases, such as skin thickening (scleroderma) or muscle inflammation (polymyositis).
Because of its overlapping nature, diagnosing MCTD can be challenging. Healthcare providers often rely on a combination of clinical evaluation, laboratory tests (including specific antibodies like anti-U1 RNP), and the presence of characteristic symptoms to confirm the diagnosis.
Learn more about Mixed Connective Tissue Disease
Causes and Risk Factors
The exact cause of MCTD remains unknown, but it is believed to involve a combination of genetic predisposition and environmental triggers that lead to an abnormal immune response. Women are more frequently affected than men, and the disease typically manifests in individuals between the ages of 20 and 40. Understanding the genetic and immunological factors at play is crucial for developing targeted treatments and improving patient outcomes.
Treatment and Management
While there is no cure for MCTD, treatment aims to manage symptoms, reduce inflammation, and prevent complications. Commonly used medications include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and immunosuppressive agents. Depending on the severity and organs involved, other treatments may include antimalarials, calcium channel blockers, and lifestyle modifications such as stress management and physical therapy. Regular monitoring and a multidisciplinary approach are essential for addressing the diverse challenges posed by MCTD.
Discover More Of Our Resources
Diagnosing Mixed Connective Tissue Disease
There’s no single test that can confirm a mixed connective tissue disease (MCTD) diagnosis, so rheumatologists rely on a combination of physical exams, blood tests, and family history of autoimmune diseases. Blood tests specifically focus on detecting anti-U1-ribonucleoprotein (anti-U1-RNP) antibodies, which is a hallmark finding in MCTD, as well as antinuclear antibodies (ANA), which are common in many autoimmune and autoinflammatory diseases. These criteria help to differentiate MCTD from other similar autoimmune conditions.
- The Alarcón-Segovia diagnostic criteria may also be used to aid in diagnosis. This requires a high titer of anti-U1-RNP antibodies (greater than 1:1600) and the presence of three or more of the following clinical manifestations:
- Raynaud phenomenon
- Hand edema
- Synovitis
- Histologically proven myositis
- Acrosclerosis
Living with MCTD
Living with MCTD requires a multidisciplinary approach, involving rheumatologists, pulmonologists, and other specialists. Regular monitoring and early intervention are crucial to managing the disease effectively. Patients are encouraged to adopt a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques.
Mixed Connective Tissue Disease is a complex condition that highlights the intricate interplay of the immune system and connective tissues. While it poses significant challenges, advancements in medical research and treatment options offer hope for improved quality of life for those affected.
Related Blog Posts
February 2, 2025
No one expects their life to change dramatically over a short period of time.