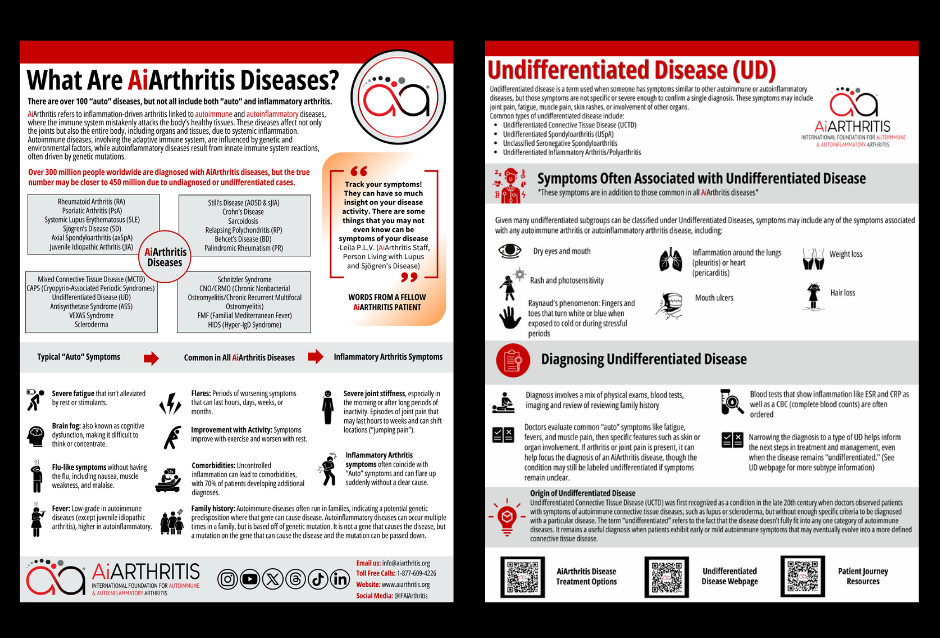
Are you or a loved one navigating life with AiArthritis diseases? The International Foundation for Autoimmune & Autoinflammatory Arthritis (AiArthritis) brings you this comprehensive guide to better understand these conditions and their symptoms. Learn about over 20 AiArthritis diseases, discover the importance of symptom tracking, and find support tailored for you.
Highlighting Schnitzler Syndrome: A Rare Autoinflammatory Disorder

Schnitzler Syndrome is a rare and underdiagnosed autoinflammatory disease first described by French dermatologist Liliane Schnitzler in 1972. It is characterized by a combination of chronic urticarial rash, monoclonal gammopathy (typically IgM), and systemic inflammation. This condition is considered a paradigm of acquired autoinflammatory diseases and poses significant challenges in diagnosis and management due to its rarity and complex presentation.
There are only about 300 or so known cases of Schnitzler in the world. Most of the reported cases of Schnitzler syndrome have been from Europe, particularly France, but cases from Australia, Japan and the United States have been reported too.
AiArthritis Disease Symptoms
AiArthritis diseases share common features such as flares, where symptoms worsen for hours to months, and improvements with physical activity, while rest can make symptoms worse. Genetic predisposition or mutations can lead to these conditions running in families, and uncontrolled inflammation often results in comorbidities, affecting 70% of patients.
Key symptoms include:
- Severe fatigue that persists despite rest or stimulants
- Brain fog, making concentration difficult
- Flu-like sensations like nausea and muscle weakness
- Low-grade fevers (higher in autoinflammatory diseases)
- Joint stiffness, especially in the morning or after long periods of inactivity
- Sudden, shifting joint pain that starts and stops abruptly
Clinical Features of Schnitzler Syndrome
Schnitzler Syndrome manifests with a range of symptoms, including:
- Chronic Urticarial Rash: Persistent hives-like rash that does not respond to conventional antihistamines.
- Monoclonal Gammopathy: Presence of monoclonal IgM (or occasionally IgG) in the blood, which is a hallmark of the disease.
- Systemic Inflammation: Symptoms such as fever, joint pain, bone pain, muscle aches, and fatigue.
- Enlarged Organs: Enlargement of lymph nodes, spleen, or liver may occur.
- Laboratory Findings: Elevated inflammatory markers like ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein), along with increased neutrophil counts.

Diagnosis
Diagnosing Schnitzler Syndrome requires a combination of clinical evaluation and laboratory tests. The Strasbourg Diagnostic Criteria are commonly used, which include:
- Chronic urticarial rash.
- Monoclonal IgM or IgG gammopathy.
- At least two of the following: fever, bone pain, elevated ESR/CRP, neutrophilia, or abnormal bone imaging findings.
Due to its nonspecific symptoms, Schnitzler Syndrome is often misdiagnosed as other conditions like chronic urticaria or autoimmune diseases.
Treatment
The introduction of IL-1 receptor antagonists, such as anakinra, has revolutionized the treatment of Schnitzler Syndrome. Anakinra provides rapid relief from symptoms, often within hours of administration, and helps control systemic inflammation. However, continuous treatment is required, as symptoms typically recur upon discontinuation.
Other treatment options include:
- Corticosteroids: May provide temporary relief but are less effective long-term.
- Immunosuppressive Drugs: Often used in cases with severe systemic involvement.
- Supportive Care: Management of complications like anemia or organ dysfunction.
Living with Schnitzler Syndrome
Patients with Schnitzler Syndrome face significant challenges in managing their condition. The chronic nature of the disease and its impact on quality of life necessitate a multidisciplinary approach, including:
- Regular monitoring by specialists in dermatology, rheumatology, and hematology.
- Psychological support to address the emotional toll of living with a rare disease.
- Patient advocacy to raise awareness and improve access to effective treatments.
Research and Future Directions
Ongoing research into the pathophysiology of Schnitzler Syndrome focuses on the role of the NLRP3 inflammasome, a key component of the immune system involved in inflammation. Understanding this mechanism may lead to the development of targeted therapies and improved diagnostic tools.
Schnitzler Syndrome is a rare but impactful disease that requires early recognition and effective management to prevent complications and improve patient outcomes. Advances in treatment, particularly with IL-1 receptor antagonists, offer hope for those living with this challenging condition. Increased awareness among healthcare providers and patients is essential to ensure timely diagnosis and access to care.
Discover the AiArthritis Equation Project - AUTO + Inflammatory Arthritis = X OR YZ, a patient-led initiative aimed at improving early detection and diagnosis of autoimmune and autoinflammatory arthritis. By raising awareness of key symptoms and promoting timely referrals, this project empowers patients and healthcare providers to work together for faster, more accurate diagnoses.