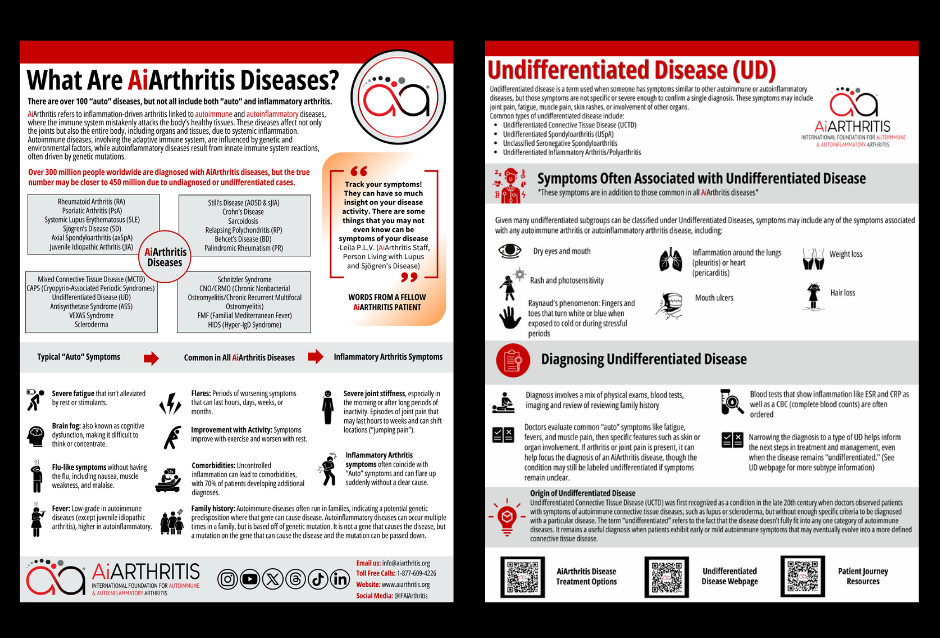
What Is Undifferentiated Disease (UD)?
AiArthritis Disease Symptoms
AiArthritis diseases share common features such as flares, where symptoms worsen for hours to months, and improvements with physical activity, while rest can make symptoms worse. Genetic predisposition or mutations can lead to these conditions running in families, and uncontrolled inflammation often results in comorbidities, affecting 70% of patients.
Key symptoms include:
- Severe fatigue that persists despite rest or stimulants
- Brain fog, making concentration difficult
- Flu-like sensations like nausea and muscle weakness
- Low-grade fevers (higher in autoinflammatory diseases)
- Joint stiffness, especially in the morning or after long periods of inactivity
- Sudden, shifting joint pain that starts and stops abruptly
Symptoms Associated with Undifferentiated Disease
Undifferentiated disease can display symptoms associated with any autoimmune or autoinflammatory arthritis condition. These symptoms highlight the diverse and overlapping nature of undifferentiated diseases, making diagnosis a complex process. Examples of symptoms could include
- Fatigue
- Skin rashes
- Dry eyes and mouth (also called “sicca symptoms”)
- Hair loss
- Mouth ulcers
- Weight loss
- Inflammation around the lungs (pleuritis) or heart (pericarditis)
- Raynaud’s phenomenon: extremities turning white or blue in cold temperatures
- Thyroid disease
- Arthritis
In saying this, UD can include any symptom from any of the 100+ autoimmune or autoinflammatory diseases, which is more than only the diseases we focus on - which narrows the group down to the couple dozen that also usually involve inflammatory arthritis as a major clinical component.
Learn more about Undifferentiated Disease
Common Types of Undifferentiated Disease:
Undifferentiated Connective Tissue Disease (UCTD)
Undifferentiated Connective Tissue Disease (UCTD) is a condition where patients exhibit symptoms and laboratory findings suggestive of a systemic autoimmune disorder or connective tissue disease, but not enough to meet the criteria for a specific diagnosis like lupus or rheumatoid arthritis. Common symptoms include joint pain, swelling, skin rashes, fatigue. Undifferentiated Connective Tissue Disease might later on be diagnosed as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), scleroderma, sjogren’s disease or myositis.
Often UCTD is a go to diagnosis under the UD umbrella, possibly because it’s studied in research more often or maybe because the diseases it may evolve into conditions diagnosed more often.
Years ago it was thought about 15% of patients initially diagnosed with UCTD evolve into a different diagnosis, but more recent studies suggest that number is closer to 35%. AiArthritis believes the number of patients who actually have UCTD - or a similar UD subgroup - is 50%, but many meet the criteria for diagnosis and go undiagnosed altogether, staying a “mystery patient” for months or years. We proved this theory to be true in 2013 during our Early Symptoms of AiArthritis Diseases, where 15% of patients initially diagnosed with UD evolved into a different disease and an additional 39% had no diagnosis but could have qualified for UD. They all evolved to an AiArthritis disease, making the prevalence 54%.
Undifferentiated Spondyloarthritis (USpA)
Undifferentiated Spondyloarthritis (USpA) refers to a condition where individuals show signs and symptoms of spondylitis, such as inflammatory back pain or heel pain and pain in other joints, but do not meet the criteria for a definitive diagnosis of specific spondyloarthritis types like axial spondyloarthritis (which includes diagnoses of non-radiographic axial spondyloarthritis and ankylosing spondylitis), reactive arthritis, psoriatic arthritis, or enteropathic arthritis (associated with inflammatory bowel diseases). Conditions, like ankylosing spondyloarthritis - but not as often with non-radiographic axial spondyloarthritis, are often associated with the HLA-B27 gene. Over time, some patients with USpA may develop a more well-defined form of spondylitis, while others may continue to experience chronic but generally mild symptoms.
Unclassified Seronegative Spondyloarthritis
Similar to USpA, Unclassified Seronegative Spondyloarthritis is characterized by inflammatory back pain, uveitis, gastrointestinal symptoms, and rashes, but without the presence of rheumatoid factor or other inflammatory blood markers often associated with AiArthritis diseases. (Negative blood markers means “seronegative”.).Like USpA, Unclassified Seronegative Spondyloarthritis can evolve into a diagnosis of ankylosing spondylitis, reactive arthritis, psoriatic arthritis, or enteropathic arthritis.
Undifferentiated Inflammatory Arthritis/Polyarthritis
Undifferentiated Inflammatory Arthritis/Polyarthritis is a term used when patients exhibit signs of inflammatory arthritis affecting one joint for 6 weeks or longer (inflammatory arthritis) or multiple joints (polyarthritis) but do not fulfill the criteria for a specific type of inflammatory arthritis like rheumatoid arthritis or psoriatic arthritis. Undifferentiated Inflammatory Arthritis/Polyarthritis may turn into a diagnosis of rheumatoid arthritis (RA) or psoriatic arthritis.
Get Involved with
AiArthritis’ Work to Improve Lives of Those Living with UD
Diagnosing Undifferentiated Disease (UD)
Undifferentiated Disease (UD) presents a significant challenge in the medical field. The absence of diagnostic criteria for many forms of UD makes the process difficult. Rheumatologists typically rely on a combination of physical examinations, blood tests (such as ESR, WBC, RBC), and imaging studies, along with a family history of autoimmune or autoinflammatory diseases.
Note: for most AiArthritis diseases, blood tests do not need to be positive, which, unfortunately, is not well known - even by health professionals.
Doctors assess common symptoms of autoimmune and autoinflammatory conditions, including fatigue, fevers, and muscle pain (myalgia). They then evaluate more specific features such as skin or organ involvement. The presence of arthritis or joint pain can help narrow down the diagnosis to an autoimmune or autoinflammatory arthritis, but the condition may still remain undifferentiated if the clinical features are not definitive.
Given that symptoms can be intermittent, it is essential to conduct tests and imaging during flare-ups to capture signs of inflammation. If this is not feasible, documenting symptoms through photos and symptom logs can be crucial in aiding diagnosis.
The Role of Rheumatologists and Undifferentiated Disease (UD)
A rheumatologist plays a crucial role in diagnosing and managing Undifferentiated Connective Tissue Disease (UCTD), Undifferentiated Spondyloarthritis (USpA), Unclassified Seronegative Spondyloarthritis, and Undifferentiated Inflammatory Arthritis/Polyarthritis. Here's how they contribute:
- Diagnosis: Rheumatologists are specialists in identifying and diagnosing various rheumatic diseases. They use a combination of medical history, physical examinations, lab tests, and imaging studies to differentiate between these complex conditions and provide an accurate diagnosis.
- Treatment Plans: They develop personalized treatment plans tailored to the specific needs and symptoms of the patient. This can include medications (such as NSAIDs, DMARDs, or biologics), physical therapy, and lifestyle modifications.
- Monitoring Progress: Rheumatologists regularly monitor patients' progress to ensure that the treatment is effective and to adjust the plan as needed. They track disease activity and watch for potential side effects of medications.
- Patient Education: They provide valuable education and support, helping patients understand their conditions, the importance of adherence to treatment, and strategies for managing symptoms and maintaining quality of life.
- Collaboration with Other Specialists: Rheumatologists often work with other healthcare professionals, such as physical therapists, occupational therapists, and primary care physicians, to provide comprehensive care for patients with rheumatic diseases
Treatment for Undifferentiated Disease (UD)
Identifying a subtype of UD can help guide treatment decisions, but even if the disease remains undifferentiated treatments should be considered. Treatment for Undifferentiated Disease (UD) focuses on managing symptoms and preventing disease progression. Here are some common approaches:
- Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. Corticosteroids may be prescribed for more severe inflammation. Other medications may include hydroxychloroquine, or steroids. Pending severity, immunosuppressive drugs might be used to control the immune system's activity.
- Lifestyle Changes: Regular exercise, a balanced diet, and adequate rest can help manage symptoms and improve overall health. Avoiding triggers, such as stress and extreme temperatures, is also important. However, lifestyle changes alone have not been proven to treat UD and subgroups - with the exception of very mild disease.
- Physical Therapy:
Physical therapy can help maintain joint flexibility and muscle strength, reducing pain and improving mobility.
- Regular Monitoring: Regular follow-up appointments with a rheumatologist are essential to monitor the condition and adjust treatment as needed.
- Supportive Care:
Counseling or support groups can provide emotional support and help patients cope with the challenges of living with a chronic condition.
Each treatment plan is tailored to the individual's specific symptoms and needs. It's important to work closely with a healthcare provider to develop a comprehensive management plan.
Related Blog Posts
September 10, 2025
Discover why being persistent is important when seeking an AiArthritis Disease diagnosis.
May 19, 2025
Chronic Nonbacterial Osteomyelitis (CNO) and Chronic Recurrent Multifocal Osteomyelitis (CRMO) are rare autoinflammatory diseases that cause bone inflammation without infection.
May 2, 2025
Discover more about this rare disease.
Show More