Decoding Biomarkers:
A Comprehensive Guide to Testing and Diagnosing
Autoimmune and
Autoinflammatory Arthritis Diseases
Types of Biomarkers for
AiArthritis Diseases
However, it’s crucial to recognize that biomarkers are just one element of the diagnostic equation. Some individuals with these diseases may never exhibit positive blood results, despite having active disease. Therefore, the diagnostic process encompasses more than just lab tests—it also includes your symptoms, clinical evaluations, imaging, and medical history. Your healthcare provider will adopt a holistic approach to understanding your condition, meaning a negative blood test does not eliminate the possibility of an autoimmune or autoinflammatory disease.
Rheumatoid Arthritis (RA)
- Rheumatoid Factor (RF): An antibody often found in RA patients, though not exclusive to the disease
- Anti-Cyclic Citrullinated Peptide (Anti-CCP): Highly specific for RA and often used for diagnosis
- CRP (C-Reactive Protein) & ESR (Erythrocyte Sedimentation Rate): General markers of inflammation, often elevated in RA
- ANA (Antinuclear Antibodies): Sometimes present in RA
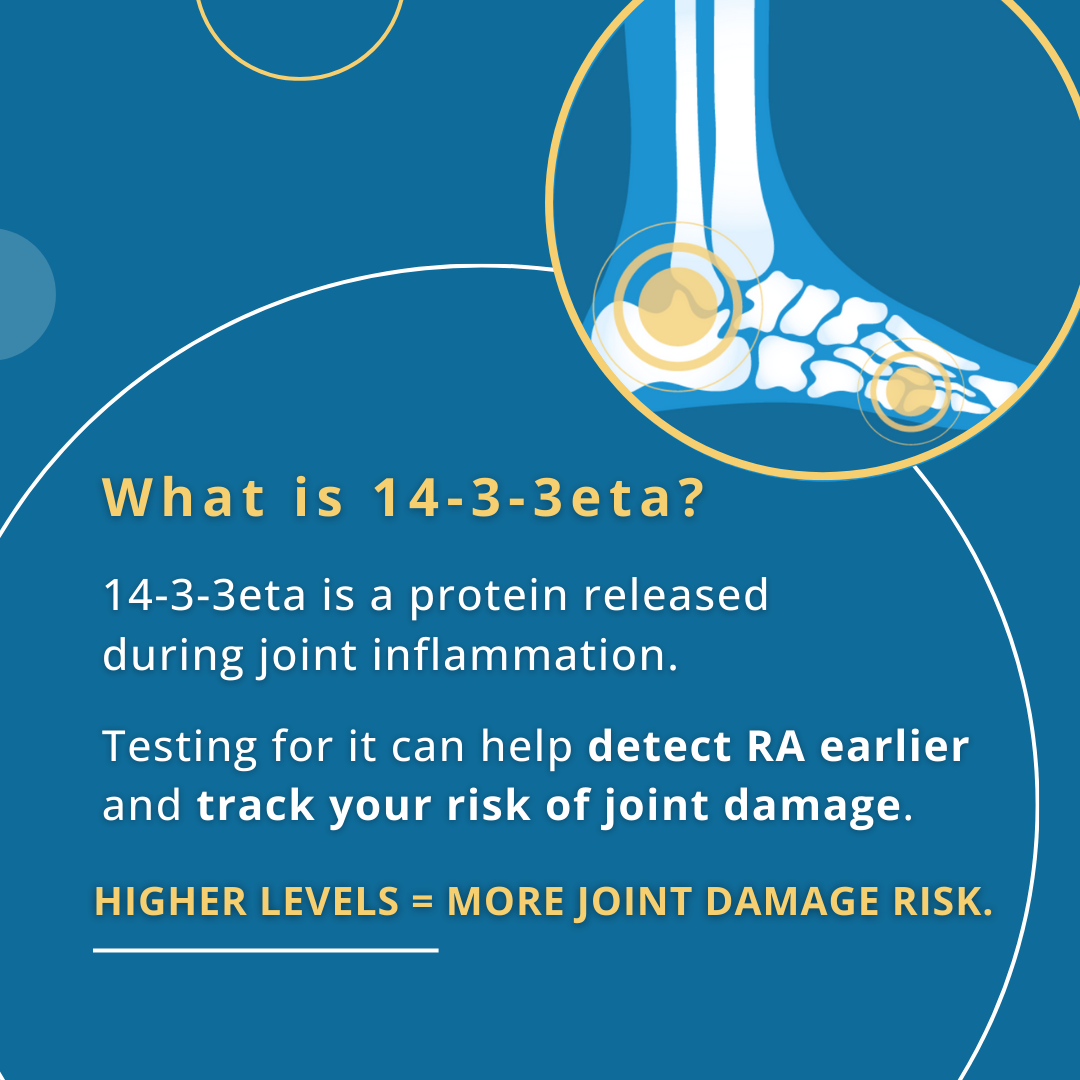
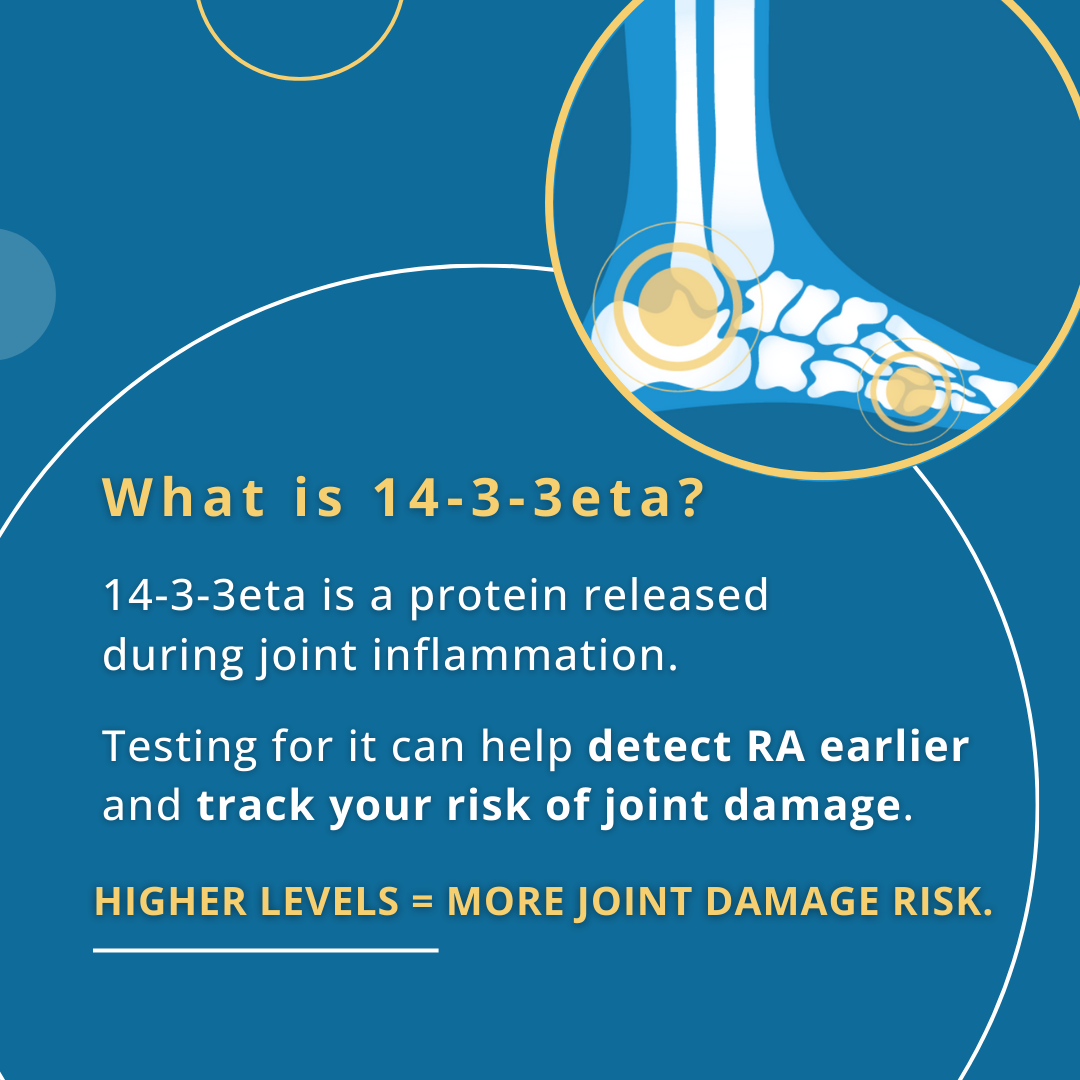
- 14-3-3eta
- In addition to RF and anti-CCP, doctors may also test for 14-3-3eta, a protein released from joints during inflammation.1 This marker is specific to RA and can help identify the disease earlier, including in patients who test negative for RF and anti-CCP (seronegative RA).2,3 14-3-3eta is also valuable beyond diagnosis, since higher amounts are linked to a greater risk of joint damage and levels tend to fall when treatment is working.4,5 For this reason, it is often used together with CRP to monitor how well a treatment is controlling disease progression and to support ongoing care decisions.4,6
References: 1) Maksymowych WP, van der Heijde D, Allaart CF, et al. 14-3-3η is a novel mediator associated with the pathogenesis of rheumatoid arthritis and joint damage. Arthritis Res Ther. 2014;16(2).
2)
Maksymowych WP, Naides SJ, Bykerk V, et al. Serum 14-3-3η is a novel marker that complements current serological measurements to enhance detection of patients with rheumatoid arthritis. J Rheumatol. 2014;41(11):2104-2113. 3)
Naides SJ, Marotta A. 14-3-3η in “Seronegative” Rheumatoid Arthritis. J Rheumatol. 2015;42(10):1995.
4)
Carrier N, Marotta A, de Brum-Fernandes AJ, et al. Serum levels of 14-3-3η protein supplement C-reactive protein and rheumatoid arthritis-associated antibodies to predict clinical and radiographic outcomes in a prospective cohort of patients with recent-onset inflammatory polyarthritis. Arthritis Res Ther. 2016;18:3. 5)
Hirata S, Marotta A, Gui Y, Hanami K, Tanaka Y. Serum 14-3-3η level is associated with severity and clinical outcomes of rheumatoid arthritis, and its pretreatment level is predictive of DAS28 remission with tocilizumab. Arthritis Res Ther. 2015;17:280.
6)
Hirata S, Marotta A, Hanami K, et al. SAT0062: 14-3-3ETA predicts joint damage progression and flaring after adalimumab discontinuation. Annals of the Rheumatic Diseases. 2017;76:791.
Learn more about Rheumatoid Arthritis
Learn more about Augurex's Work in Rheumatoid Arthritis
Check out our 14-3-3eta Informational Graphic Below & On Our
Social Media Platforms

Slide title
Write your caption here
Button
Slide title
Write your caption here
Button

Slide title
Write your caption here
Button

Slide title
Write your caption here
Button

Slide title
Write your caption here
Button
Slide title
Write your caption here
Button
The Importance of Biomarker Testing
Biomarker testing plays a significant role in diagnosing and managing autoimmune and autoinflammatory diseases. However, it is only one aspect of the diagnostic process. While these tests offer valuable insights into your condition, it is crucial to understand that not all individuals with these diseases will have positive blood work. Therefore, doctors consider a comprehensive view, including your symptoms, physical examination, medical history, and imaging results, when making a diagnosis.
If you experience symptoms indicative of an autoimmune or autoinflammatory condition, it is essential to work closely with your healthcare provider to explore all diagnostic avenues. By understanding the role of biomarkers and their place in the broader diagnostic process, you can feel more empowered and informed about your health journey.
Discover More Of Our Resources
Why Some Autoimmune and Autoinflammatory Diseases Lack Biomarkers
While biomarkers are incredibly useful in diagnosing and monitoring many autoimmune and autoinflammatory diseases, some conditions lack specific biomarkers that clearly indicate their presence. This can complicate the diagnostic process. Here’s why this happens:
- Complex Nature of the Immune System: Autoimmune and autoinflammatory diseases result from complex disruptions in the immune system, which vary widely among individuals. Some diseases do not produce specific, detectable antibodies or other measurable markers that can be easily identified in the blood. For instance, conditions like Behcet’s Disease or Relapsing Polychondritis lack unique biomarkers. Diagnosis often relies on clinical symptoms and the exclusion of other diseases rather than specific lab results.
- Overlapping Symptoms: Many autoimmune diseases share similar symptoms, such as joint pain, fatigue, and inflammation, making it difficult to distinguish one condition from another through biomarkers alone. Diseases like Undifferentiated Disease (UD) may present with symptoms across multiple conditions without fitting neatly into one diagnosis, complicating the identification of specific biomarkers.
- Variability in Disease Expression: Autoimmune diseases can vary greatly between individuals. While one person may have detectable biomarkers, another person with the same disease might not. In diseases like Sjögren’s Disease or Lupus, some individuals might show elevated antibodies, while others with the same diagnosis might not. This variability can be influenced by genetic factors, disease stage, or the presence of other medical conditions.
- Lack of Specific Research: For some rarer diseases, such as Schnitzler Syndrome or Systemic Juvenile Idiopathic Arthritis (sJIA), the scientific community may not yet have identified a clear biomarker because the disease hasn’t been studied as extensively as more common conditions like rheumatoid arthritis or lupus. Research is ongoing, but in some cases, we simply don’t have enough data to establish a reliable biomarker.
- Disease Processes Not Linked to Antibodies: In some conditions, the underlying disease process may not involve the production of specific antibodies or other measurable proteins. For example, axial spondyloarthritis (particularly the non-radiographic form) often does not produce detectable antibodies. Instead, the disease is diagnosed through clinical evaluation, imaging studies like MRI, and the presence of certain genetic markers like HLA-B27, which may or may not be present.
Learn More About Biomarkers on AiArthritis Voices 360 Talkshow
Diagnosing Without Biomarkers
The absence of a specific biomarker does not mean a disease cannot be diagnosed. Physicians rely on a combination of other diagnostic tools, including:
- Clinical Evaluation: Your doctor will assess your symptoms, medical history, and physical exam findings to look for patterns that suggest a specific condition.
- Imaging: Techniques like X-rays, MRIs, or CT scans can help visualize inflammation, joint damage, or other structural changes linked to certain diseases, especially in cases like Ankylosing Spondylitis.
- Symptom Patterns: The timing, frequency, and combination of symptoms help narrow down the diagnosis. For example, recurrent episodes of fever, joint pain, and rashes may point toward periodic fever syndromes like Familial Mediterranean Fever (FMF).
- Response to Treatment: Sometimes, doctors may trial certain treatments to observe how a patient responds. A positive response to a treatment targeting autoimmune or autoinflammatory pathways can further confirm a diagnosis, even in the absence of biomarkers.
In these cases, diagnosis becomes more of a process of exclusion—ruling out other conditions through various tests and narrowing down the possibilities based on the overall picture of symptoms and disease behavior.
While biomarkers are valuable tools in diagnosing many autoimmune and autoinflammatory arthritis diseases, they are not always present or conclusive. Some diseases are simply too complex or individualized to produce consistent biomarkers. Understanding this helps patients and healthcare providers focus on the bigger picture—looking at symptoms, clinical evaluation, imaging, and other diagnostic methods to arrive at a diagnosis. If you’re navigating a diagnosis without clear biomarkers, remember that your healthcare provider will work with you to piece together all the information available to make the most accurate diagnosis possible.
Related Blog Posts
April 22, 2025
From the essential role of vitamin D to groundbreaking findings on exhausted T-cells, this research is shedding light on ways to better understand, manage, and treat autoimmune conditions.
April 22, 2025
Menopause is a significant, often under-discussed phase of life for patients with rheumatic diseases. The insights shared at ACR 2024 highlight the importance of comprehensive, patient-centered care.
April 22, 2025
Exploring New Research: Transforming Lives Through Better Understanding and Treatment
Show More