REWIND: Differentiating Arthritis & Autoimmune vs Autoinflammatory
AiArthritis Voices 360 Main, Full Episode 91
Air Date: November 5, 2023
This episode is a Step 5, as outlined in our 6 Step Patient-Led Problem Solving Process.
This is an AiArthritis Voices 360 REWIND, where we are bringing back two short episodes that were recorded way back in 2019, because chances the topics are very important! Also note - you will hear the acronym IFAA, which we used prior to using AiArthritis.
The first segment revisits an episode where Tiffany is joined by Dr. Apostolos Kontzias to explore the distinction between autoimmune and autoinflammatory diseases. In the second segment Tiffany discusses the importance of differentiating between arthritis types to improve the misunderstandings that are associated with arthritis and, in turn, will help expedite detection.
Join us in this episode discussing AiArthritis’s mission to improve awareness and understanding of these conditions.
Episode Highlights:
- Innate vs adaptive immunity
- The difference between autoimmune and autoinflammatory diseases as well as the subcategories such as age and onset
- Why Stills Disease needs two brochures, juvenile onset and adult onset.
- If patients do not have positive labs or biomarkers, it does not mean they do not have an autoimmune disease
- Listening to your patients is important because every patient is different.
- Importance of doctors and nurses understanding of the different types of arthritis diseases to increase early detection.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient co-hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide to solve the problems that matter most.
Whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table.
[00:00:45] Tiffany: Welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation Autoimmune Autoinflammatory Arthritis.
We just say AiArthritis for short. My name is Tiffany Westridge-Robertson. I am the CEO and original founder of the organization. And like all leaders at AiArthritis, I also am living with AiArthritis diseases. My primary diagnosis is Axial Spondyloarthritis or non-radiographic version if you wanna be really detailed about it.
And we've got kind of a, a flashback, I guess we're going to be doing. We realized we're, we've hit a hundred some odd episode and there's so much content that we have that we know many of you either have never heard or you heard it three years ago, and you probably don't remember, and so we also were looking into the projects and programs that we have coming up in the very near future and realize a few of our shows really do set us up in preparation for what those are going to be.
So those are the ones we're going to replay for you all today. In saying that, what are these programs and projects that you speak of, Tiffany? Well, let me tell you. Okay, everything we do at AiArthritis, whether you know this or not, is based on what patient's report is missing. That's how our whole organization was founded, actually.
We united with a bunch of patients online, and we all started talking and having aha moments. Well, the first one being there needs to be a non profit that focuses only on the autoimmune and the auto inflammatory arthritis diseases. And the thought was that well, hey, if we narrow it down to just those 20 or so that are these auto diseases with the inflammatory arthritis that we just narrowed down from like a hundred plus of autoimmune and auto inflammatory diseases.
So there you go. Perfect example of ever since then same plan, we listen to each other, we talk, we have aha moments and patients decide, you know what, if only this happened, maybe we could improve lives. So, one of the things we've been wanting to do for years is pre is work on earlier detection diagnosis or referrals and guidance.
And so we are going to be launching a program called Auto Plus Inflammatory Arthritis Equals X or YZ. And this is going to be a program that will highlight the typical autoimmune and autoinflammatory features of disease that typically will happen regardless of your diagnosis, plus an inflammatory arthritis and what makes that different from your more traditional osteoarthritis or gout or other types.
Then, if you have those, plus that inflammatory arthritis symptoms, that is highly likely, or likely, I shouldn't say highly, I'm not a doctor. It could be, it could be that you have one of our diseases, so that is that. And then we also picked a couple diseases that we felt were, even though they don't necessarily fall under the Aiarthritis disease umbrella, they are strongly related to our diseases, one being what is called IgG4. That is something we have talked about quite a lot here on the show. And we are, it is a related disease, it's often been diagnosed alongside many of our diseases. So Sjogren's syndrome, sarcoidosis, lupus, rheumatoid arthritis but definitely in the wheelhouse. And then another one, fibromyalgia, which is not an autoimmune disease, which is often misunderstood. It is a nerve condition, and it is quite often either originally diagnosed and then re-diagnosed with one of our diseases, or many people have dual diagnosis, so that would be Ry and Rc that we chose.
So to do that, a couple of things I mentioned here, one is we would like to be able to differentiate that arthritic component, so the inflammatory versus the mechanical or the degenerative when you've got aging, the more common kind. So that's gonna be a real big feature here. So differentiating our greatest types and why that's so important.
And then another component is really zeroing in on this education of what is an autoimmune disease and what is an autoinflammatory disease. A lot of times people leave the autoinflammatory out of our name. When they say the full name, but not just AiArthritis , they'll often cut it down to autoimmune and inflammatory.
And there are such things as autoinflammatory diseases. They are not as common as autoimmune. They are often rare diseases. The ones under our umbrella are, so for example, Stills disease, systemic juvenile idiopathic arthritis, which is also called Stills disease. That's just the juvenile version, Bechets disease, sarcoidosis. So just to name a few, we do have several rare diseases under our umbrella, all are auto inflammatory. And that is really a difference in where in the immune system, the disease originates. One is you are innate meaning you were born with it. Another is learned or acquired. And so that dictates what it's going to be labeled as.
But often, as you can only imagine, it's your own immune system so things cross, right? So there's a lot of science about, well, it could be auto inflammatory, but it triggers the autoimmune. It's autoimmune, but it triggers the auto inflammatory. So no shocker there, right? But, we want to make sure that that is part of this whole project.
So without further ado, we thought let's go back to the beginning. Not quite number one, but I think it's like episode two and three, like we're in the, in the five here and we're going to do the importance of differentiating arthritis types and we're going to replay an interview style conversation that I did with Dr. Apostolos Kontzias and it was at the American College of Rheumatology, and we talked about the difference. And so we will replay that for you, and I just want to make a disclaimer. Back then we use the acronym I F A A. We no longer use that. We use AiArthritis, but if you hear me say that, that's why. So we're going to have Ryan, our producer, audio producer, tee that up for us and then I'll just be back to close it out.
So the topic we're going to talk about today is the need to differentiate arthritis types and why is this important? We believe doing so will improve the misunderstandings that are associated with this disease and in turn will help expedite detection of the autoimmune and auto inflammatory diseases where arthritis is a major component.
We also think that by addressing this and creating educational materials that it can help the conflicts and relationships that currently exist because of these misunderstandings of what a person really is dealing with. And then eventually, both of these things will improve a person's quality of life.
It can improve their health outcomes and then if that happens well, we could actually start to improve the overall cost of health care around the world. And wouldn't that be fantastic? So let's get down to the conversation here. Why do we want to do this? And what are we trying to achieve? At the root of the problem is that over many, many decades, the word arthritis has only been associated as an umbrella term, meaning joint inflammation or joint pain.
And that's what it is but the problem is that there are different types of arthritis. And if the general public only assumes that arthritis is something that is a part of aging or it happens in a mild form, oh, it's just something that I can take an over the counter product and I'll feel better. That is doing a disservice for the people who really are suffering with the various types of arthritis, whether that be the more popular osteoarthritis or our types, which is the arthritis associated with having an autoimmune or an autoinflammatory disease, we like to call AiArthritis. So the fact of the matter is we all have points of reference. We know what we know. So if we think of the word arthritis, what comes to mind? I mean, you might say, Hey, I, I have arthritis. I have it in my knee or I got it from an injury. That can happen really at any age or maybe you have the typical aging that just happens naturally and all of that falls under degenerative arthritis, which is osteoarthritis or the most common form of arthritis.
And even with saying some of those things that I just mentioned, it does come with this assumption that it is a minor situation, a minor inconvenience that might not be that painful. But the fact of the matter is even within that type of arthritis, it can be extremely serious to the point where the cartilage has worn away and it is bone to bone.
And that, of course, is extremely painful. So even in osteoarthritis, I want to make it really clear by differentiating we are not in any way, shape or form suggesting that one form is worse than the other. They all have variations of severity. But the reason we want to start differentiating in our arthritis types stems from the misunderstanding of the word.
So the first issue is relationship conflicts. So think back to a situation that you were misunderstood and it's frustrating, right? You say, oh no, you have to understand and you can jump up and but it's frustrating but you get over it, right? The next day everything is okay. Well, what if that happened every day or close to every day? Because that's the reality for people living with AiArthritis diseases. People say ugh, I'm so sick of people thinking that my arthritis is this mild form and I'm too young to have this.
I mean, there's just so many things that occur with the frustration surrounding being misunderstood in general. But then it's deeper than that because the other thing that's different about our arthritis type is that these are part of an autoimmune or an auto inflammatory disease. There are over a hundred of those, but only a handful actually present with most patients with arthritis as an early clinical component. And that's important to note because this happens at a cellular level and the inflammation travels through the bloodstream and it'll attack the joints, tissues, organs, full body and the pain that's felt is from initial onset. So as soon as that cellular level activity in the immune system starts to interact, we're feeling that pain.
Now it's going to take months and often years before any damage occurs, that anything could be seen on a radiographic image. So what happens is this invisibility, combined with young onset mind you, 20 to 40 years of age, typical of onset in adults and then you're looking at any age in children, so you've got invisible, it's not showing anything on radiographic images, all must be in your head, you're too young to have this.
So, that in itself not only causes conflicts in relationships and misunderstandings and what a person is experiencing, but it blends into point number two. And that is that if general practitioners, family doctors, hospitals, nurses, kind of a first line intervention, people don't understand that there is a difference it can extremely delay detection, and when you delay detection, you delay diagnosis, you delay therapy, and then a person could have a compromised quality of life, less chance for remission, and that's when the healthcare costs really soar. So you can see how understanding the differences can really change the paradigm of many facets of our healthcare system, as well as the people living with these diseases.
I know when I was first going to doctors to seek out advice on what was happening with me, I had a typical autoimmune features, which was fatigue. I had a fever for four and a half weeks straight that wouldn't break. I was exhausted. I was very short of breath and winded feeling like I had the flu and that's what was focused on the systemic, the full body things.
And everybody kept ignoring the arthritis. We thought at IFAA when we founded the organization, wow, if we just focus on this small group of diseases and we can educate practitioners, if somebody shows up with these symptoms that are classic autoimmune or auto inflammatory, and they have arthritis, wow, could we expedite detection and put that whole motion forward. So the things that we are asking for your help on would be your ideas on how we can create better educational materials to educate not only our family and our peers and our significant others. But also medical practitioners and the public, because think about it, if anybody listening has one of these diseases, before you became affected, you were the public.
So if you as the public knew about this type of arthritis, maybe you would have gone to a doctor earlier. So it all really feeds off of each other.
So, those are the things that we're looking for your feedback on because we are ready to change the stories of tomorrow and it all starts with education. Don't forget to visit our podcast page at AiArthritis.org/podcast where you can meet some of our future co hosts, meet our production team, learn more about this podcast and what we're trying to achieve.
And, of course, we're always looking for your support, so learn about ways that you can donate and support our podcast to keep this alive. We appreciate it to all our existing VIPs who support us monthly and make things like this happen. Today, I actually don't have a fellow patient co host with me because we are going to share with you an interview that we did at the American College of Rheumatology, or ACR, annual scientific meeting that we as an organization attend annually. While there, we have the opportunity to speak with many stakeholders about different topics that are important to our community, and this was one of those circumstances. So, this is a great example of how we would like to utilize the podcast to include all people living with the diseases from around the world so that while we cannot afford to bring you all with us to the conferences, we can bring the conferences and the conversations that we have there with you.
So, in this episode, we are going to focus on the topic of what is auto inflammatory? What is autoimmune? What is the difference? So, I mean it's right in our name, International Foundation Autoimmune Auto Inflammatory Arthritis. There's a lot of questions, particularly in our patient community. What is the difference?
What do I have? Even our patients are a little confused and understandably so. This is the beginning of a longer conversation. This is something that's important to patients, first of all, who doesn't want to know exactly what they have. So I think that's the obvious one. But additionally, these autoimmune diseases and autoinflammatory diseases, and again, we only focus on the handful that also include arthritis as a major clinical component early on at IFA.
We do not focus on the hundred plus. However, the auto in the name does mean immune mediated, so it is about the immune system. So both types are a result of the immune system. It's just different sections of the immune system that are stimulated. And you're going to learn a little bit more about that topic when you listen to the interview that I was able to have with Dr. Apostolos Kantzias from the Renaissance School of Medicine, Stony Brook University. Dr. Kantzias was wonderful and willing to speak with us. And I asked him specifically, would you open the door to the discussion so that we can begin helping people understand a little bit about the history of how even autoinflammatory came into the conversation prior to just a couple decades ago, it was mainly autoimmune so that you will learn about. We also wanted to just get a general idea of what the differences are and how that relates to early detection, to symptoms, to research, and what we could do to help continue the conversation. So we wanted to speak with him in hopes that he could shed some light in addition to the differences between autoimmune and autoinflammatory.
But a little bit about the history and how auto inflammatory broke off in research and, and disease etiology, and also how it impacts research, early detection, patients. So this is a discussion that really needs further clarification and further conversation. But this is step one. So I'm going to let you listen to the wonderful interview we had with Dr. Kantzias, and then I'm going to circle back and talk about some highlights and ideas of how you could get further involved. Okay. Well, hello everyone. We are talking right now with Apostolos Kantzias. Did I do it?
[00:19:17] Dr. Kontzias: It was great. You've been practicing it very well.
[00:19:20] Tiffany: I have. I really have because that's a tough one.
But, I'm so excited to finally meet you in person.
[00:19:27] Dr. Kontzias: Absolutely. My pleasure.
Because we have been collaborating on a patient reported Stills Disease brochures project. That's exactly right. And that's how we met. Because I emailed you and said, we want the best.
You be the judge.
[00:19:44] Tiffany: You, well, actually it was funny because last year we told him this earlier last year, when we were here, or it was the year before I, one of them, and you were speaking and we couldn't go cause it was a paid session and we almost stalked, I, we almost stalked you outside, like,
[00:20:00] Dr. Kontzias: I could have given you tickets.
I wish I knew.
[00:20:02] Tiffany: Well now I know, now we know. But, you're at Stony Brook.
[00:20:06] Dr. Kontzias: That's exactly right. I've been with Stony Brook over the past a year and a half where I'm directing the fellowship training program there. And at the same time, I'm co directing the adult auto inflammatory clinic. And prior to that, I was six years at the Cleveland Clinic where I actually directed the adult auto inflammatory clinic there.
In my experience with auto inflammatory syndromes and patients with Stills disease and other auto inflammatory syndromes stems from my clinical fellowship years at the National Institutes of Health, where Dr. Kastner and all sorts of other, you know, world renowned scientists and clinicians, where they're seeing patients from the States and all around the world, with all sorts of kinds of auto inflammatory syndromes, especially stills as well.
So this is where all my clinical interest comes along and stems from.
[00:20:59] Tiffany: Okay. All right. Well, we're glad because I, you know, in the rheumatology world, as you know, there are very far and few in between in general, but when it comes to auto inflammatory and stills and some rarer diseases. It's even more difficult.
[00:21:13] Dr. Kontzias: This is exactly right. No, absolutely. And, patients oftentimes, they see multiple physicians, even rheumatologists, pediatric rheumatologists, infectious disease doctors, hematologists, in search of an answer to their questions and to their, to end their diagnostic odyssey there. And, we're happy to try to, you know, provide some input and, and educate both patients and physicians alike so that they can recognize, you know, signs of these rare conditions.
[00:21:45] Tiffany: Well, it's one of the things that you, that you just mentioned, it's a great segue into why I begged you to come over here and speak with me. And that is because people in our community, I mean, we as a nonprofit, we cover autoimmune and autoinflammatory diseases that have arthritis as a major clinical component early in onset.
In saying that, there is still a big confusion, particularly among the patient community. What is autoimmune? What is autoinflammatory? Which do I have? What is the difference? Could you shed some light?
[00:22:20] Dr. Kontzias: Absolutely. I'll try, I'll try my best and see how it goes. So essentially, everybody has known over the course of years, you know, what autoimmune conditions are.
And classic ones are lupus, rheumatoid arthritis, and they are related to issues with one of the two arms of our immune system and that's called the adaptive immune system as opposed to the older version of it all that we have which is called innate immune system and Dr. Kastner was actually the one who coined the term auto inflammatory to showcase the patients who have inflammatory symptoms, that is, you know, fever, rashes, joint pains and aches and arthritis, in the absence of specific signs, objectively, in primarily in the labs of conditions like lupus and rheumatoid arthritis are autoimmune conditions.
So, in patients with lupus and, and all, and related conditions. There are biomarkers, there are labs that we do for patients, you know, an ANA, double stranded DNA, rheumatoid factor, people will know that they're frequently positive and by default they are positive and that's why they are called autoimmune.
But in auto inflammatory syndromes, all of these labs are pretty much unremarkable or low positive, even though they can be highly inflammatory, these patients. And that's why there's a diagnostic delay because the markers are negative, even though there is inflammation there, people are really drawn into all kinds of different of doctors to try to figure out, you know, what exactly is going on.
But they do present both auto inflammatory and autoimmune with arthritis oftentimes. So they do have some common features with increased markers of inflammation. And at the end of the day, this was a mental construct and, and, and dichotomy for researchers and clinicians to allow grouping patients into distinct different categories so that we can study them because they do not behave the same clinically.
And they do not present in, in similar ways, necessarily, right? That was one of the major drivers behind the classification and distinction between autoinflammatory and autoimmune to begin with.
[00:24:44] Tiffany: Okay. So there are essentially, if we're trying to relate this to patients, two different sections, segments of the immune system, relating from the immune system.
[00:24:55] Dr. Kontzias: That's exactly right.
[00:24:56] Tiffany: And one being innate.
[00:24:58] Dr. Kontzias: Correct.
[00:24:58] Tiffany: Does that tend to happen to younger people because it's innate or?
[00:25:02] Dr. Kontzias: That's a very good point. In the classic type of auto inflammatory syndromes, which may be genetically mediated, you can definitely see them in, in, early on in, in children, but more and more so, we do see unrecognized, you know, patients in the early adulthood or, you know, juvenile patients, adolescents, and so on and so forth. So not necessarily, the answer is you have adult onset still disease, for example, which is a classic, you know, auto inflammatory condition that is definitively, by default, seen in patients in early adulthood, usually, or later on. And others, you know, we've diagnosed patients with TRAPS, TNF receptor associated periodic syndrome, in adults.
Maybe not as commonly as is in children, but they're out there and it requires a high level of suspicion and not assume that these are conditions of childhood or, you know, that's the key thing.
[00:26:00] Tiffany: So as far as, the other side, the adaptive, is that what the word is?
[00:26:05] Dr. Kontzias: This is what it is adaptive immunity. Yes.
[00:26:07] Tiffany: Now, and that is typically then autoimmune, correct? And some patients have asked this question, so I'm going to take this opportunity. Does there have to be an environmental component to adapt? I mean, is that what that means?
[00:26:22] Dr. Kontzias: Usually there are triggers to generate inflammatory symptoms and environmental triggers may trigger either the innate or the adaptive immunity.
[00:26:33] Tiffany: That's great.
[00:26:34] Dr. Kontzias: Yes. For example, sun exposure. I mean,
[00:26:37] Tiffany: it's not great, but you know what I meant. That's great to know because that is a misunderstanding.
[00:26:43] Dr. Kontzias: That's exactly right. Sun exposure, which is environmental stimulus, right? Trigger. Induces, triggers lupus, which is an autoimmune disease, right? Viral infections, for example, at times induce and trigger auto inflammatory syndromes, you know, such as hyper IgD syndrome.
Patients are very well aware of what the triggers are. Their menstruation, for example, or symptoms increased or triggered around menstrual cycle in women, for example, right So, this is so very important to listen to patients because every single patient is going to have a potentially different trigger and different constellation of symptoms. Even though the big picture may, may be similar overall.
[00:27:27] Tiffany: Exactly. Well, that's, that was extremely helpful. I have one more breakout question on this. One of the other things that has been transpiring over the last few years is a bridge between autoimmune and auto inflammatory. And I know myself living with spondylitis, that has come up with the question, is ankylosing spondylitis purely autoimmune?
Is it a, a scale, but I heard it last year in EULAR for lupus.
[00:27:56] Dr. Kontzias: That's exactly right. So this is an excellent, this is an excellent point. And that brings home the message that any kind of immune mediated condition can have contributions from both adaptive and innate immunity. So certain kinds of symptoms, let's say inflammation of the lining of the heart. That's known as pericarditis, right? Or inflammation of the lining of the lungs, known as serocitis or pleuritis. That can happen in both autoimmune, lupus, let's say, or autoinflammatory conditions, stills, for example, right? It's more and more known that certain kinds of symptoms have contributions from both.
And serocitis may be more of an innate immunity, auto inflammatory related symptom, as opposed to a classic autoimmune symptom related to adaptive immunity, for example. And there is anything in between, like such as spondyloarthritis, or ankylosing spondylitis, for example. By definition, you don't have autoantibodies.
Patients do not, their immune systems, in autoinflammatory syndromes, they do not recognize structural components of, of their cells, of their immune cells and others. That's by definition what autoinflammatory means.
[00:29:13] Tiffany: Okay. So, one of the things that IFAA does, literally, or part of our mission is utilizing patient voices to impact change, whether that's in education or awareness and advocacy or public policy or research. So as we're moving forward in understanding and teaching the patient community about the autoimmune versus auto inflammatory. What would you suggest to IFAA that we ask patients to report on, or to track, as far as this is auto inflammatory, or maybe this is more on the autoimmune, is there anything that we can do as a, as a patient voice, or as a non profit to specifically track, to help differentiate one or the other?
[00:29:57] Dr. Kontzias: In terms of symptom recognition, at times systemic inflammatory symptoms such as, especially fever, could be high fever, you know, could be potentially low grade fever associated with rashes, for example, that these are a couple of clinical symptoms that definitely point towards more auto inflammatory.
It's not that they cannot be seen auto immune, but...
[00:30:20] Tiffany: Like with lupus.
[00:30:22] Dr. Kontzias: Correct. Exactly. Exactly. So, lupus is a great mimicker of anything, of everything.
[00:30:26] Tiffany: Well, in psoriatic arthritis, but that's a different level. That's a different type of
[00:30:30] Dr. Kontzias: Correct. But highly inflammatory symptoms, especially in the absence of specific positive labs.
[00:30:37] Tiffany: Okay. Yeah, that makes sense.
[00:30:39] Dr. Kontzias: And increased markers of inflammation. Mm hmm. That's, that's, these are a couple of points that can give clues for both patients and treating physicians that this could be it.
[00:30:51] Tiffany: That's great. Thank, thank you. Well, before we, we wrap up here, I just want to ask you, you're here at the ACR.
[00:30:58] Dr. Kontzias: Yes.
[00:30:58] Tiffany: And, I know that you're not speaking.
[00:31:01] Dr. Kontzias: Not, not this year.
[00:31:01] Tiffany: See, and shoot, I could have got it now, we could have got it for free. So next, either EULAR or ACR, I'm going to stay tuned, but tell us just a couple of exciting things that you plan on doing while you're here.
[00:31:15] Dr. Kontzias: Yeah. So, so I'm planning to review posters in regards to recurrent pericarditis, that's, that's one of the potentially autoinflammatory conditions presenting both in children and adults.
There's a high burden of disease activity in these patients and what do we do with steroid dependent and cortisone resistant for these kind of patients. So there are a couple of interesting posters there. There are a couple of very interesting talks from the group, the NIH group of Dr. Kastner and Dr. Umbrello, Mandy Umbrello. Who's going to be giving a talk on patients with undifferentiated autoinflammatories. And so how do you approach?
[00:31:55] Tiffany: I saw that. Is that a paid one?
[00:31:57] Dr. Kontzias: I think so. Maybe, maybe.
[00:31:59] Tiffany: Maybe we need to talk.
[00:32:00] Dr. Kontzias: Maybe, yes.
[00:32:00] Tiffany: Because I think I had that on my list and now I'm like, oh.
[00:32:04] Dr. Kontzias: Both are excellent speakers.
[00:32:07] Tiffany: Okay. You might get a text from me later.
[00:32:11] Dr. Kontzias: Yeah. So, so, yeah, it's a very interesting conference to attend to.
[00:32:16] Tiffany: Okay. Well, great. Thank you so much too for coming by and doing this.
[00:32:21] Dr. Kontzias: Appreciate it.
[00:32:22] Tiffany: Wrapping up here with Apostolos.
[00:32:25] Dr. Kontzias: Yes.
[00:32:25] Tiffany: I'm not even going to do the second one. I, I got through the first one.
[00:32:29] Dr. Kontzias: You're good.
[00:32:30] Tiffany: All right. Thank you again so much.
[00:32:31] Dr. Kontzias: I appreciate it much. Thank you.
[00:32:32] Tiffany: All right, well, I'm back and I hope you enjoyed that conversation. Thank you again, Dr. Kontzias for taking your time out at the ACR to have that conversation with us. We greatly appreciate your time and willingness to help our community. I think that lends to a great start to further conversation and breakout discussions that will be very relevant for our community and for the stakeholders involved in our community.
So a couple highlights that I found quite interesting and I feel that would be interesting to continue the conversation with and that was autoinflammatory being considered a young disease. We at IFAA are currently working on a patient reported stills disease brochure project. And that means we are talking to patients to get their input.
I can't tell you how many patients said, I really think we should have two different brochures. Now, for those who aren't familiar with Stills Disease, researchers and doctors will tell you that the biology is the same, regardless if you have childhood onset or adult onset. So the science says no, you don't need to have two brochures.
You have one brochure for Stills Disease. Why would you have one for juvenile onset or adult onset? Again, because the science says they're the same, but this is important to note because patients don't say it's the same. Some of them don't have opinion on it, but the ones who do have an opinion and some strongly believe that there are presentations that are different because of being a child and because of being an adult and we are definitely going to explore those. Because that is very relevant to understanding how the disease in this case could differentiate not only between autoimmune and autoinflammatory, but within childhood to adulthood. So that's a whole breakout section to discuss. But the point of this is, he mentioned, it's not just a child's disease.
And the second reason that we have been asked to do two different brochures is because I have heard story after story of patients who say, I went in as an adult. I was in the hospital, out of the hospital, extreme flares, pushing my stomach in because the pain was so intense, I could not sit up straight.
The fevers were so high, I was waking up in the middle of the night with these extreme sweats, feeling completely like I had the flu, hot flashes, and nobody was listening because when I brought up stills, or if the subject of stills came up, I was told, you're not a child, you can't possibly have this disease.
We can't let that continue to happen and it's not just still we're using that as an example because we are working on that project right now and Dr. Kontzias used as an example as well. He's actually our advisor on the project so hence now you see the connection there. But the point is, is that not only do we need to understand the differences between autoinflammatory and autoimmune and the different subcategories, age, onset, for example, but we need to understand that autoinflammatory, which is often thought to be young onset and often it is young onset.
We cannot forget that there is a patient population being forgotten and that's just not okay. So, that is one thing I wanted to pull out of that. One other thing I wanted to point out that I think warrants further investigation is the fact that auto inflammatory tends to present with extremely high inflammation that travels directly to the body in an intense way, causing extreme flu like symptoms, and it can affect organs very early on. So, it's not relying on any type of trigger of the immune system to then go back and attack. It is innately attacking. So, it comes on very aggressive. It does not always present with positive blood work or laboratory results or biomarkers, which are more common to use for diagnostic criteria in autoimmune diseases.
However, while I did not break out to explore that topic while I had Dr. Kontzias because of limitations on time, and it opens the door to a whole new conversation, which we will have now. I'm not sure who the other stakeholders will be at the table, but this is definitely a conversation we need to have.
There are so many autoimmune patients who do not have positive labs and do not meet the biomarkers and they are told you don't have this disease. Thankfully, there are many rheumatologists today that understand you can still have autoimmune diseases and not have positive labs or biomarkers. I want to point that out because if it is something that's being considered in the medical community as a differentiating factor between autoimmune and autoinflammatory, we don't want some practitioners to believe, well, it must not be autoimmune because you don't have the biomarkers or the positive labs.
So we certainly want to continue our work to monitor that. The overall takeaway was a quote when he said, listen to patients, everyone can be different. And how relevant is that? That's the exact reason why we do this podcast, because we know at IFAA that while persons who advocate, we advocate, we're, we're out there speaking, we're only a small percentage of people.
We cannot possibly speak on behalf of all people and that's why we're doing this podcast so that we can reach as many as we can and let you know you have a voice. And doctors, as Dr. Kontzias said, it's important to listen to the patients because everyone not only can be different, I'm going to say is different and our stories matter. So, this is the opening conversation for autoimmune versus autoinflammatory.
Well there you go. So I'm excited to bring back some of these episodes. We're going to do this a couple more times too, just to make sure some of this amazing content that we have doesn't fall off and it's repurposed and reused, especially as we start to go through this process that we do at AiArthritis, which is we put a topic on the table and then we go back and we work and we come up with other ideas and then we put it back on the table when we're ready to produce a project or a program or resource. And tah-dah here we are, what a great example. So I'm putting those two topics on the table as we did a couple of years ago.
Now, here we are ready for this program. So you can check out all of these other episodes that we had at our website, aiarthritis.org/talkshow. And while you're there, we certainly would appreciate a donation. Your support does help us keep this going. And we would love to hear from you. So send us a message, visit us on social media at IFAiArthritis on all of the platforms and looking forward to really getting this project going.
If it's something that you might be interested in and getting involved in in some way, helping us create the materials. That's right. We do bring our volunteers on to help with those kind of things too. Go ahead and click to volunteer and let us know, hey, in the comments in this section, when you're talking, I heard this talk show in this really cool project, auto plus inflammatory arthritis equals X or YZ and I think I kind of want to be involved in that. And we'd be happy to bring you on as always, as we stay only together, we truly change the stories of tomorrow. And that is no different here today. So thank you so much for tuning in until next time.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www.AiArthritis.org. Also, be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.
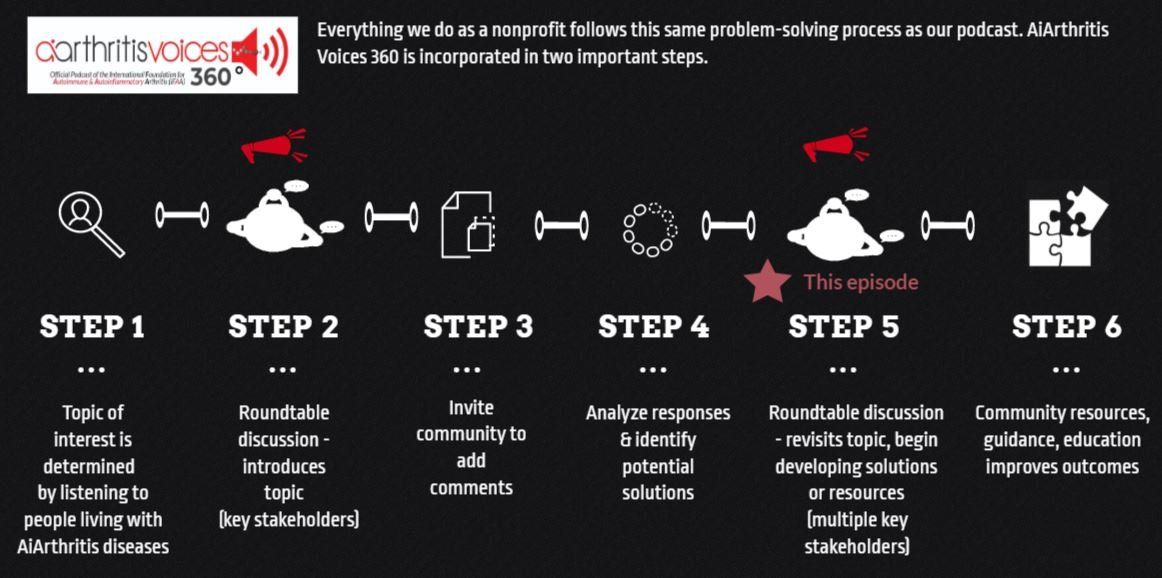
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!
Your Host: Who is at the Table this Episode?
Tiffany Westrich-Robertson
Tiffany is the CEO at International Foundation for AiArthritis and uses her professional expertise in mind-mapping and problem solving to help others, like her, who live with AiArthritis diseases work in unison to identify and solve unresolved community issues.
Connect with Tiffany:
- Facebook: @tiffanyAiArthritis
- Twitter: @TiffWRobertson
- LinkedIn: @TiffanyWestrichRobertson
Dr. Apostolos Kontzias
Dr. Apostolos Kontzias is the Vice Director, Center of Autoinflammatory Diseases at Stony Brook University, Renaissance School of Medicine. Dr. Kontzias is one of the national and international experts in the field of autoinflammatory diseases/periodic fever syndromes. His subspecialty interest includes seronegative spondyloarthritis and Sjögren’s syndrome.
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Episode #2: Typical vs. Atypical: Which are you and why does it matter?
This episode join your host, Tiffany, as she and co-host Deb Constien discuss the challenges faced by patients who experience atypical disease presentations, especially the need to advance our understanding of this phenomenon because the typical is not so typical.
Episode 3: Autoimmune vs. Autoinflammatory: What's the Difference?
This episode join your host, Tiffany, and special guest Dr. Apostolos Kontzias from the Center of Autoinflammatory Diseases, as they discuss the distinction between these two sides of the immune system.
Auto+Inflammatory = X or YZ
Patient-led project aimed to increase detection, referrals, and diagnosis.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.