Surgery with an AiArthritis Disease
AiArthritis Voices 360 Main, Full Episode 89
Air Date: September 3, 2023
This episode is a Step 2, as outlined in our 6 Step Patient-Led Problem Solving Process.
Tune in to the latest episode of AiArthritis Voices 360 Talk Show, where your co-hosts Leila, Deb, and Kerry candidly share their personal journeys of undergoing surgery while living with AiArthritis diseases. In this episode, the co-hosts delve into their surgical experiences, including the pivotal surgeries they've had due to their conditions. From Deb's journey triggered by a bunion removal to Kerry's hip replacement due to the complex interplay of autoimmune conditions or Leila’s gastric sleeve surgery due to weight gain from treatments, the trio reflects on the unexpected intersections of surgeries and AiArthritis diseases.
They discuss the preparations they navigated before surgery, the challenges they faced with doctor clearances and insurance, and provide valuable insights for fellow AiArthritis patients, including the crucial questions to ask healthcare professionals. Listen in to gain a unique perspective on surgeries with AiArthritis diseases and discover firsthand the resilience and strength that arise from these experiences.
Share your questions here:
info@aiarthritis.org
Episode Highlights:
- What surgeries each co-host has had and whether they are related to their AiArthritis disease
- What preparation is required before surgeries with an AiArthritis disease
- What questions patients should ask their doctors to prepare for surgery
- Co-hosts share their recovery journey
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you
all to the table where together we face the daily challenges of autoimmune and auto inflammatory arthritis. Join our fellow patient co hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide to solve the problems that matter most.
Whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table.
[00:00:53] Leila: Alrighty, welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and
Autoinflammatory Arthritis, or AiArthritis for short. My name is Leila, and I am the Health Education Manager here at the organization, and a person living with SLE and Sjogren's disease.
Today, I am joined by Kerry and Deb, who are both long time AiArthritis volunteers. and recurring co hosts on the AiArthritis Voices 360 talk
show. If you wanted to go ahead and introduce yourself, Deb.
[00:01:27] Deb: My name is Deb Constien. I am in the Madison, Wisconsin area and I have had RA since I was 13 years old. So a long time, 40 plus years. Kerry, how about you?
[00:01:43] Kerry: Hi, everyone. I am Kerry Wong, also known as the butterfly from FloatLikeAButtahfly. I am in New York, Westchester County, New York, just about a minute north of the city, and I am livingwith what my rheumatologist likes to call autoimmune soup, so that's got
a primary base of a rare disease called sarcoidosis, and it's got some extra seasoning from rheumatoid arthritis and Sjogren's as well.
[00:02:10] Leila: Alrighty. Well, I, I always love how you explain that's so visual that you can kind of picture a soup there with all of the different
diseases. I didn't get to mention that I am also living in Southern California. So we have the East Coast, the West Coast, and the middle of the U. S. represented here today. I love it and so we do have a very interesting topic for you all today. We will be discussing having surgery while also having an AiArthritis disease. There may be, you know, a multitude of reasons for why you might have surgery while having an AiArthritis disease, but we have noticed that there are a few common threads when preparing and recovering from surgery. And we also wanted to make sure that we put out a disclaimer that these are our personal experiences and stories. And that we are not medical experts or giving medical advice, but more of just telling our own stories to connect with you, whether you're having surgery upcoming or you've already had surgery.
And so, let's get started. Okay, let's start out with what surgeries did we get, surgery or surgeries, and what was the reason? Deb, did you want to start?
[00:03:23] Deb: Sure. Since it's been 40 plus years, and a lot of my time, probably 15 to 20 years, was pre biologics, so a lot of not great
medications, so it didn't keep me in really good control.
I'm kind of fixing what the first 20 years allowed. I guess, I guess I would call it my very first surgery, which was when I was in high school. It was a freshman in high school. I had a bunion removed from my right foot, and that is what essentially triggered my RA. So ever since then, I've been a very different person, I would say. I've had two cervical neck fusions, a wrist fusion, total knee replacement on my left side. During COVID, I had reconstructive foot surgeries on both feet, about 10 months apart from each other, which was a hard pill to swallow because that was not a fun time. But I guess my husband was home, so he's like let's get her done. Not relating necessarily to my RA, but I've also had Hysterectomy, and I've had ovary removed because I left my ovaries and one ovary went crazy, so I had to have it removed and I think that's it. So most of my disease, or most of my surgeries have been RA and AI disease related and the very first one being kind of the hologram of, ah, that's what kind of kicked off my disease. So sad to say, but again, I think it's made me the person I am and I'm a stronger person for it, so.
[00:05:20] Leila: Absolutely. I think talking about triggers of autoimmune diseases also such as Interesting topic. So that's crazy that that's what
triggered your RA. I've never heard that story before. So that's why I was like, oh my goodness.
[00:05:33] Deb: Yeah, it literally what I literally went into the hospital the day after Christmas to have the surgery and I came home such a very different person. Everything hurt. And it snowballed a huge, like, storm in my body, so I was immediately referred to a rheumatologist at that point.
And at that time, they didn't have pediatric rheumatologists, so I saw an adult rheumatologist. Luckily, he was close enough in my area, so it wasn't that big of a deal. But it was, that was a tough time, because everything hurt, and they were again, the medications weren't really good back then. So, it was a lot of trial and error, and a lot of error.
[00:06:24] Leila: Yeah, and you were 13, you probably just wanted to go play basketball, or go run and dance with your friends, and things like that, so.
[00:06:32] Deb: And I, I didn't, because I only had enough energy to go to school, come home, do my homework, and I kind of went into a bit of a bubble because my friends would ask me to do things and I would often say no because I just I didn't have any more energy. It was an energy sap sucker at that point. So, it kind of sucked.
[00:07:00] Leila: Yeah, definitely. Kerry, did you want to talk about your surgery?
[00:07:04] Kerry: Sure. So I just, I have to say, you can't see it right now, but my mouth literally dropped Deb, when you said about having that one triggered, your autoimmune disease and everything kind of since, because I, I had not heard that and it just, my mind is kind of spinning because I'm thinking about how long I've been sick and surgeries that I've had and I had mentioned earlier I had a bunch of surgeries back in 2008 2009, and none of them had anything to do with this because I wasn't chronically ill. I wasn't in the, you know, AAiArthritis world at all.
But I'm wondering now if that is what actually triggered it, was having a number of gynecological surgeries including hysterectomy also back in 2008. And I spent the next four years trying to figure out what is wrong with me. What's wrong? I have all these things. And so I'm just, you know, my mind is blown right now that I really have to go back and look at things and think about how much
[00:08:18] Deb: there's a lot of correlation. Yeah, there's a lot of correlation. They say it can be a severe car accident, a surgery where exposing your, your inners so to speak. And
[00:08:44] Kerry: I have not, and that is just wild, but that was not the surgery I planned on talking about today. So the surgery that I just had
about two and a half months ago, and I am still, you know, recovering from is I just had a hip replacement, a total hip replacement. And while technically in some ways, you might say that that's not really from AiArthritis. I's from, I had very severe degenerative arthritis or osteoarthritis, which is different and I had developed avascular necrosis, which is basically where the bone begins to die because it's not getting the blood or the oxygen that it needs to survive. And so those don't sound like they're AiArthritis related conditions, but the reason that both of those developed is because I was put on steroids as soon as they saw I have some kind of arthritis.
And so I spent over 10 years on steroids and with that, you know what, probably most people listening in have at least that love, hate
relationship with steroids, but you know, two of the really big side effects that they cause are weight gain and weakened bones. And that's a really, really bad combination.
And so with over 10 years on steroids, I gained over a hundred pounds. And my bones got weaker and weaker. And so I just had my, my hip replacement and I got to tell you, I love my new hips so much, and we can get into that a little bit more, but yeah, so that's really what I had and so it's technically not AiArthritis, but it really is. And so it really is, it's that combination. There is the systemic inflammation, there is the joint inflammation, all of those things that just kind of pour onto each other and say, this is not good.
[00:10:56] Leila: Absolutely and now here sitting, listening to both of your stories. Now I am going to expand on what I was going to talk about too. Because, so the original surgery that I was going to talk about, and I'm still going to talk about today, is I got gastric sleeve surgery about two months ago, and that is a bariatric surgery, a weight loss surgery to basically help those who can't really get weight off on their own. And I always say that. You know, my, I have been big my whole life, but I also was put on prednisone for the first time when I was eight years old. And when I was in fourth grade, I gained 50 pounds on prednisone as a fourth grader.
And from then on, I just never lost any of my prednisone weight either. So every round that I went on prednisone, I always gained more and more weight which therefore caused me to get to the point where I am now, where my starting weight was 360 pounds. So I was, you know, at that point where I'm like yeah, this something has to change. Not only because of my lupus is my, are my joints always hurting, but because of the weight that I have on too. And so it's been on my radar to have this surgery since I was 18 years old. So, so for almost 10 years, I finally got into the place where I felt my lupus was in remission for long enough that I could get an elective surgery. I was in a financial place where I feel like I have enough money security to be able to take off a few weeks from from work and and do all those things and also in a mental health space where I was ready for this challenge because a lot of people may see gastric surgery as an easy way out.
That's what all you know, a lot of people in the community talk about and it's actually so much harder than anybody could even imagine. So, that's the surgery that I'm gonna focus on because that's what recently happened. But, the only other surgery that I've ever had in my life was, right after I was diagnosed with lupus, I had a slipped hip. Well, actually, both slipped hips. So, it, the term that they call it is skiffy, but it's like a slipped cap of your hip. So, it's like this, and my, the bone of the top of my, of the cap of the joint was like this. So it was where the cap was showing. They, yeah, they said that if they were to put it back in place, that there was a risk of damaging nerves. So what they did was just put a screw through it. So I have a screw this big through my left hip. The right one wasn't slipped enough for them to do the surgery, but it was slightly slipped. It's just like a storm of things that happened. It probably had to do with the prednisone that I was on for a very long time.
It also has to do with the fact that I was just getting my period and become like going through puberty. So my joints were still flimsy, they weren't fused, they weren't like, you know, as strong as they, as they usually are when you, after you hit puberty, that's when your bones are like fully fused and things like that.
And also it happens a lot to the Asian Pacific Islander community, especially when you're younger. So all of those things were just the perfect storm to cause that surgery to happen. Ironically enough, my mom had just given birth to my little sister in the same hospital. So we went home on the same day with my crutches and my little baby sister with her cheeks just jiggling up and down as we were driving home. So, my poor mother, I don't even know how she survived it except for she had to bring me to my grandparents house for two weeks to go stay there because she just had a new baby. But yeah, so those are my two surgeries that don't have to do with AiArthritis disease, but do have to do with AiArthritis disease also. So yeah, I didn't, I didn't even think about talking about my hip surgery, but I, now that I think about it, it probably was. Contributed to to with the the steroids. So wow, it's that the synergy of our stories is just so weird
[00:15:13] Deb: Yes agreed and it always natural conversations that just happen for sure
[00:15:18] Kerry: Definitely and you know talking about the idea of even you know of having the weight loss surgery that also has so much, you
know, it's like all with, you know, with gaining so much weight, all my doctors have ever said was that, you know, oh you have to lose weight.
You have to lose weight. And like okay I would, if you'd give me something else that wouldn't make me keep gaining. And I had a few of the doctors then suggest that I get weight loss surgery also, and I because this was, that was the only way I was going to be able to lose weight, but I even met with a bariatric surgeon who told me ultimately I was not a good candidate for the surgery, that there were, I think, two different types that we looked at, the bypass and the sleeve, and I won't remember which is which, but one of them I would not be a good candidate because I'm on so many other medications for all these other conditions that I think it was the bypass that my body wouldn't absorb all of the medication that I take if I had that done. And the other one I think was that it would increase risk of or severity of other issues that I had already. And so, you know, it's because of all of this that I should have it, but it's because of all of this that I can't.
[00:16:44] Leila: Absolutely, and going off of that, maybe I can kind of like slide us into the next topic of preparation for my surgery. Because that's one of the biggest things is qualifying for the surgery. So with a BMI of over, I think they say a BMI over 30, you already qualify. My BMI was like 56. So that was, it was, it was not a question of whether or not I qualify for the surgery, but if I, my body could handle it in terms of my lupus and everything like that.
And one thing that they didn't tell me until the week beforehand is you cannot take a pill bigger than your pinky nail, but this my pinky nail isn't a good representation right now because I have nails on but this is how small the medication is supposed to be that you're supposed to be able to swallow after surgery. I was on kidney medication that was this big, all of my magnesium yeah, magnesium supplements are huge multivitamins are huge and so I started freaking out like a week before the surgery because I was like what am I going to do with all my medication and they told, they all told me, I think you're, you're a little too scared about what's going to happen.
We will figure that out when it happens, because in order to play around with the medication, they have to see the blood work and see how I'm doing afterwards. And so long story short, I ended up getting off of all of my blood pressure medications and all of my kidney medications because of how well the surgery worked for me. After the first week, I was feeling light headed, and I was like, why am Ifeeling so light headed? Like, I can't get up without feeling dizzy. It's because my blood pressure was tanking because I was taking my medication and so, my doctor was like, yeah, just stop taking it. I'll see
you in a week and she was like, yeah, your blood pressure is completely stable it was one week after the surgery.
It was like it felt like magic that it just happened all of a sudden. So that was part of the prep was for my insurance we had a three month course that we had to go through I had to go through cognitive behavioral therapy and I had to go through nutrition classes, and I had to do an exercise program. That's not necessarily for every surgery, but for insurance to cover it for
me, that's what I had to do. Mine was completely covered by insurance because I was able to go through all those steps. But I do know people who have gone to Mexico to do it because it's easier and they don't have to do all those requirements and it's, you know, $5,000 to go do it there or there's another type of surgery that's not as covered by insurance called the duodenal switch, which is a newer technology that is also you have to pay for out of pocket. So that one is about $12,000. So I am very lucky and very fortunate that I have the insurance that I do have now. Like I said, it was all just like a perfect situation for me to be able to get the surgery done for that I'm very thankful. And yeah, I had to get clearance from my rheumatologist, but she said she had no qualms of, of me doing the surgery.
I've been in a clinical remission for about two years now. She was like, you know, this is the perfect time. And also it ties into me wanting to start, you know, family planning soon too. And so, we all felt like it was the best situation for me to get the surgery done first so that I can be healthy enough to house a little baby. So that's a little bit about my preparation. The reason, like I said, was because of how heavy I got a lot due to the prednisone and a lot due to being in so much pain to not be able to work out the way I would want to but yeah I think the the preparation in terms of my AiArthritis disease was just making sure I was in remission long enough to withstand the the big change on my body.
[00:20:42] Deb: That makes sense, that makes a lot of sense. As far as my preps go each one of them was A little different, but historically the biggest thing that was required of me each time was that I had to be off my Celebrexo anti inflammatory medications, and I think it's for full week
before you even have surgery. And, I also had to be off my hormones because of my severe hot flashes. So, I had to go off of my Premarin and the Celebrex and there was other tweaking with, it seemed like with each surgery and also requirements. Some surgeries, they required that I have an EKG and I have my chest x ray and all these other different procedures, all the to
again, have all your ducks in a row prior to having surgery and seeing, so now that, of course, with all the other problems I'm now seeing a cardiologist and all of those things.
So it, it snowballs in you having to touch base and again, managing your own care. You need to make sure you're touching base with every one of your doctors so everybody has equal input because when I had my knee replacement, my surgical pain management was horrendous and it was to the point where I cried for about 48 hours straight because they would give me nothing more than a Percocet or a Vicodin I'm like, can you please look in my chart to see that I am NOT a standard patient and that was probably the worst part of it, and as far as preparation goes, that, and again that part of that recovery was horrendous, and it definitely empowered my husband, because my husband could only spend so much time in my room, because I was just bawling, and PT and OT would come into the room and walk right back out, they're like, we can't even touch her, and again, not doing really good things for my joints and everything like that so. Those are some of the things that I had and it is mostly because of all the medications that were on and tweaking things and making sure that they're keeping fine tune of blood pressure. That was another thing during covid, I had both feet reconstructive foot surgeries done and my blood pressure was incredibly high and i'd been talking about it for a long time. I'm like this is not normal, and I'm like, I don't want to have a stroke, because it was close to 200 over 108, and they, I mean, I could have stroked out, but they kept saying, oh but you're in pain. I'm like, yeah, I'm always in pain. That, that isn't a reason for my blood pressure to be that high, which caused eye damage, and now it took over a year and three medications later, that now I've got my blood pressure under control, but now I'm seeing a cardiologist because of all the other issues that happen. Gotta love it. And we've got to, yeah, we've got to be really big advocates of ourselves too and again, not take no for an answer. I kept getting poo pooed, even though I kept bringing it up, and it wouldn't show up in my follow up notes. And I'm like but we talked about it! That's kind of like a really quick synopsis of some of my stuff that I had prior to surgery and like preps and things like that.
[00:24:47] Kerry: That's the perfect place for me to kind of piggyback into mine, is that idea that you have to be an advocate for yourself. You
cannot take no for an answer when you know that something is wrong. Trust that. And if the doctor that you see doesn't want to listen, and the
doctor that you see doesn't want to act, then that is when it's time to find another doctor, because no one is going to look out for you better than you.
And no one knows what's going on inside your body better than you do. And so, you know, again, talking about eligibility and preparation and clearance leading up to surgery, the hardest part was getting a doctor to do it. Because I had been told, initially, I was told I was going to need to have a hip replacement, but not yet. And I asked the doctor, well, what determines when? And he said, when it's so bad that you can't take it. And I said well, if I could take it, I wouldn&'t be here. And he said well, when it gets worse for now, maybe you'll just get, you know, a steroid injection. And I spent a year and a half going to, you know, we tried the injections, we tried pain management, we tried physical therapy, back to another doctor, to another, back and forth and around again. In the meantime, I had broken my foot twice, and I believe that part of that is because I was so unsteady because of this horrible hip that was in so much pain. So I liked the orthopedic surgeon who was dealing with my foot. So I asked him about my hip and he initially said that he could talk, he could see me for my hip.
And then when I had to make a separate appointment for my hip because we couldn't discuss it in the same visit as we were, we were there to look at my foot. But when I went back to him, what he did then was refer me to another orthopedic surgeon who is sometimes better able to work with people who are heavier. And I said, okay, and I got excited because this one was going to help me. He wasn't putting it off until it gets worse. It's just a matter of it's not his thing. Here's someone who could do it. And I went to see this other orthopedic surgeon and we looked at my x-rays and he was so great in
how he educated me. He had my X-ray up on his screen, and he showed me where, you know, the differences were from the good hip to the bad hip. He showed me where there were cysts in the bone, and where there was degeneration of the bone. And he showed me what the procedure would entail in order to fix it. And then he told me he wouldn't do it because he would not do it. So after all of that, what I thought was the perfect visit, he then said no, and I, he would not do it. And again, there's that BMI factor, and he said he would not do it for someone whose BMI is higher than 40. I said, but if we don't do it, it's only going to get worse. And he said, well, then you need to lose weight.
And I said, well, how am I supposed to lose weight if I can't move? He said well, have you thought about surgery? I said, yes, I have and I wastold I'm not eligible. And he said, all right, well, why don't you come back and see me in three months and maybe if you've lost weight by then, we'll talk about this again. I was heartbroken. I was devastated because the visit started off so good. And I went home and I cried and I screamed and I yelled some things that I will not say on this broadcast and what was really, I will say what was really, really great was I posted about it on Facebook and when I posted about it on Facebook, I had so many friends in the arthritis and AiArthritis community who some just empathized and I needed that some offered suggestions.
I had a number of people who said, if you need to, my friend has a doctor she loves. And one of my friends actually told me about her doctor and she had recently had her knees replaced. And she also had had a hard time finding someone to do it because of her weight. And she said, but this guy did it and she loves him and he's great. And when I went to see him we talked about everything and he put in my file, in my chart, in my chart for every other doctor that accesses it to see. He specifically said that yes, I need to lose weight, but we don't see how that's possible until I'm able to move. And I was just like, oh my God, thank you so much. When he left the room just to get a schedule, my mom was with me, and the two of us were crying in his office because we were just so happy that he said yes. We scheduled it out, I had a couple of dates, like two months until it happened, and then all the surprises came. And that's when I found out that I couldn't just go and have surgery on this date.
I had to get clearance from my primary, my rheumatologist, my neurologist, my cardiologist, and I think there was one other ologist that's just, oh, did I say rheumatologist? Maybe. Yeah, I think my pulmonologist also, because the sarcoidosis is this systemic inflammatory thing, and it also affects the lungs, so we had to make sure everything, everywhere, everyone said, okay, and even that, of course, couldn't be that simple because then the cardiologist who was filling in for my regular cardiologist who was out on leave, so because this one didn't know me, she wanted to run extra tests and so I also had to have the chest x ray and I also had to have an ultrasound and a CTA, which is like a CT of your arteries and then we had to wait on all of that and I was literally down to like three days before surgery, crossing my fingers, hoping that the results came back and everybody would say, okay. And in the meantime, I also had to stop my infusions. I get, I get ID infusions for small fiber neuropathy, which is how the sarcoidosis affects my nerves. I get infusions every week. I had to stop that for a month. I had to stop one of my other medications that was my Imurin. I had stopped that for a week before and after. I had to stop a couple of other things. And now I was stopping all of these medications without even knowing whether or not I was going to be able to have the surgery. Fortunately, everything worked out. My tests were good enough to let me go and I was able to have the surgery and I am so, so, so, so glad that I did.
[00:32:40] Deb: Yeah, every one of my surgeries are again, blessings and I look back and I'm like, why did I wait so long and so long it was because people wouldn't give, my knee replacement was before I was 30 years old. So, that is not, that is again, highly unusual because doctors don't want the liability and they also don't want the wear and tear with the weight and all of that on the joint. So they're thinking, well, I'm going to have to go back in there in 10 years and do another one. And so again, there, it's a blessing when you can get the right doctors, the right team, the right, everything, all the ducks in a row. And you feel like crumb going in for surgery because you feel, you're in pain. I mean, you're uncomfortable. You're really uncomfortable with where your meds are.
[00:33:37] Leila: Yeah, absolutely. I, a lot of mine had to, my recovery, like the beginning of the recovery, had to do with missing my infusion also because I am, I am so reliant on Benlista. It's like my best friend. And I can, like, anytime that I have to stop it, it's like, It's like a disaster in my brain because I'm like, I don't know what I'm going to do. I've been on it since 2014, so this time around, it unfortunately, it was, so I had to push it back a month after my surgery, and I had gotten it two weeks before my surgery, so I was out of it for six weeks total, and usually I start hurting like four or five days before my next infusion, so while I was recovering, the biggest thing that they tell you to do is walk, walk, walk as much as you can, and that, it was, and that's the hard thing is that when you, you have a when you have a minimally invasive surgery, in order to do that, they fill your stomach up with gas so that there's, there's so much more visibility. And in order to walk off that gas, that's the only way you can get rid of it is by walking and doing all those things. On top of that, I had my surgery in the summer and with lupus and all other, other AiArthritis diseases, there's sun sensitivity involved. So I was like, like so in so much pain and I'm like, I gotta go put on sunscreen before I go walk and all these things.
But, I was able to still do maybe about 10 minutes at a time walking. But because of the lack of the infusion, I was having a lot of fatigue. And that
was probably the hardest part, the also what I forgot to mention in the prep and also it had to do with recovery was I was on a liquid diet for four weeks, so two weeks before the surgery and two weeks afterwards, and the two weeks afterwards was a lot harder than the two weeks before, just because I was like, so determined to do it because of the surgery. And once the surgery happened, I was like, I am literally drinking Gatorade and chicken broth and I just want to eat something again so that one that was the like a really tough part, but I think it also at the same time prepares you for What is coming next when you can eat food. Because a lot of people do end up getting the surgery because they are addicted to food. They have a relationship with food where, you know, anything goes wrong in your life and, and you, you eat and when you're happy, you eat. When you're sad, you eat, when you know anything happens. When, especially in the culture that I grew up with as a Filipino, as an as an Asian American, everything is surrounded with food, you know, anything that you do, there's big buffets everywhere and things like that. So a lot of my family was like, oh, I don't know how you're going to do it.
Like you love the buffets, you love all this food and things like that. And I was like, but I love living a lot more than those things. So I'll figure it out. So I am eight weeks out now. I am currently able to eat solid food. The thing that a lot of people, don't know and are surprised by is that my doc, my surgeon advises me to just eat protein. There's no veggies or fruits involved, carbs are you know, stay away from it as much as you can. Because for veggies and, and fruit, everything that's beneficial from them you can get from multivitamins. Of course, it's always better to eat the whole foods, but they recommend that you spend all of your stomach space on protein because there's not too much that you can supplement protein with. I mean, whey protein is still not as good as the actual protein from meat. So a lot that I've been eating is like shrimp, salmon, and I am able to eat beef. For some reason, my stomach is not tolerating chicken, which is really weird. Because that's one of the first meats that they recommend you eat. But every time I eat chicken, it hurts my stomach. But right now I'm able to eat maybe about four, four ounces of food at a time. So about this much food I'm able to eat, or let's say like the size of a coaster. That's like the amount that I'm able to eat at a time less than a thousand calories a day.
But what I am most excited about is that I am officially 43 pounds down. So I am, I'm at 327, sorry, 317 and so my big celebration I'm super excited to do is when I, once I get under 300, because I've not been under 300 since maybe 2017, 2018. So that will be super exciting once that happens. Otherwise in the recovery, I think the biggest thing that I was struggling with was the tinkering of the medications and just waiting to figure out what was going to happen because, so I stopped all my medications that I had to before surgery and I was on a very delicate balance of supplements, specifically, I have always gotten recurring UTIs. And so I had to always take a women's probiotic every day, and once I got, I didn't prepare enough before surgery to have all of the bariatric supplements, like the stuff that my body could actually absorb, I didn't have it until maybe a week and a half after, so right after surgery, I got a UTI, and when you get a UTI, you're supposed to take antibiotics, and the antibiotics that they gave me were really big, and also made my stomach upset, and so even to this day, I'm still fighting with the infection.
Like it's coming in and out, like UTIs are just the worst. And you know, when you take antibiotics for UTI, then you develop a yeast infection. All these different things. It's just such a hard balance to keep. So, I think that, that was the hardest part was just dealing with the repercussions of adjusted medication or stopped medication and supplements. So, also I had a headache for 10 days because I wasn't taking my magnesium supplement. And I didn't figure that out, that that was the reason why until recently when I accidentally didn't take my magnesium supplement and I had the same headache that I had in the beginning of my recovery and I was like, that is why I had such a bad headache.
I guess my, my cervical area is just so used to having the magnesium that when I don't have it, I get an extreme tension headache. So even to this day, I'm still learning so much about my body and what it needs to function optimally, and as an arthritis patient, I think we're always learning that, and new things that can help us be at our highest optimal like, you know, functioning, so, yeah, that was, that was a little bit about my recovery, the biggest thing that it affected, it didn't affect my AiArthritis disease, I was praying that it would not cause a flare or anything like that. I think that's always the scare for us is you just never know what's going to happen when you come out of there and how your immune system is going to act. So yeah.
[00:41:21] Deb: Agree. But I also think again, I think the three of us are really blessed with great partners. I've got my husband of almost 30 years. You've got your fiance. Kerry, you have your husband. I think we all have amazing, supportive partners, partners in crime, you know, that just help support and know what to say and what to do kind of help you mentally get through some things too. That's one thing I think, you know, having a great support system.
[00:41:56] Leila: And also not making you feel bad for not being able to do things. I think that is the biggest thing that I would, that like, I would
not be able to live with is if, like, you know I'm going to have a surgery, then don't be upset that you have to take up some extra chores, you know?
[00:42:12] Kerry: Yeah, I, I agree with that a hundred percent. It, it definitely makes a world of difference, to have someone who understands and empathizes, and even if they don't know what to do, they're ready to sit there and say, how can I help you? That is huge. And I, I don't know how I could get through it if I didn't have him. That said, because of course, a lot of, you know, there are plenty of people who are watching this who don't necessarily have a mic on their side right there. I want to refer back to what I was saying earlier that when I was so frustrated about that doctor who wouldn't help me and I went online and there is such an incredibly strong support community, through AiArthritis, through social media, that even if it's not somebody who lives with you and is willing, is able to do the dishes when you can't, you can definitely get that support, all around.
And I also just want to say, Leila, I am so happy for you. I'm so proud of you, you know, what struck me was, you know, when your family said, well how are you going to do that because you like to eat? And you said, because I like this. I like living more. And that's as basic and obvious as that sounds, that is a really, really difficult statement to make, and it's really, really hard to get to that point. And so the fact that you did, and that you followed through, and that you're seeing such a good result from it I am just, I'm like beaming with joy and pride for you and so I had to say that, and while we're on the beaming with joy, I have to say, and, and surgeries that went well. So I am, you know, after my surgery, I had for a couple of weeks, physical therapy at home, occupational therapy at home, nurses coming to my home and other than like a week before it started.
I didn't know any of that was going to happen. But you know, I've since progressed to physical therapy, outpatient and I am so amazed with the difference that this new hip has made and, you know, I love my physical therapist. She works me hard, but it's, it's so paying off. I, I literally every day, I'm just like, I can't believe the difference that this makes. And, you know, a couple of you may have seen, I posted on Facebook the other day that I, for the first time, was able to walk around outside. I went out for brunch with my husband and a couple of friends and I went to the car and I went from the car to the restaurant and around the restaurant and back to the car and back to my apartment and I did all of that without a cane, without a walker. I'm still afraid to go out without it, without bringing my cane with me, and, and part of that is because although I did just get a new hip, I still have RA, and Sjogren's and sarcoidosis, and all of these things can flare up at any time. But for the first time in eight years, I was able to go out and not use a cane, and it was just amazing. So while I will still always have it with me, or maybe not always, my physical therapist suggested maybe just keep it in the car.
But, so I know that there are still all these other things I'm dealing with, and, you know, getting back to infusions, and getting back to medications, and getting back to all of those other things, you know, I'll sometimes joke that, you know, that something is doing better because there's some other body part that's screaming at you a little bit louder. But you know, the best thing that I can say right now is, and I just have a lot of fun saying it because I'm a dork and I like wordplay, but I will paraphrase Jay Z and say that I've got 99 problems, but a hip ain't one.
[00:46:55] Leila: Yeah, I love that. I actually too, I just, past two weekends, I went to a concert and I went to a baseball game and I walked 8, 000 steps and 11, 000 steps and I, I swear to you, before 2019, like, I haven't done, not done that before, until before 2019 and so, and Joseph, my fiancé, was like, you didn't, you didn&'t ask to stop once, you didn't ask to take a break you didn't, you know, need to go wipe off your sweat and go take extra water while we were walking and he was like, he's like, I'm so proud of you. I have, I, I've, that hasn't happened in so long. And I was like, I'm proud of myself too.
[00:47:38] Deb: I love it. Yeah. Seriously, it gives, it gives you like, it gives you your life back in certain ways. Again, I, I, I remember the fear of going in for my cervical neck fusions. And again, the second time was almost worse than the first time because I knew what I was going in for. And just everything as far as all of those pieces, but again, you get a piece of your life back when surgeries go right and go well. So, that is kind of like what I stand by, is just sometimes you gotta grunt through it and get her done, but the reward on the other side is so much better.
[00:48:24] Leila: But yeah, I think that overall just hearing the stories of all of the different surgeries, you know, there's gonna be a lot that comes
up especially with AiArthritis disease mostly having to do with joints but there there are other things that come up and I think you know, we want
to give a few just like pointers. We've kind of been sprinkling out it out throughout the episode too but I just wanted to, open the floor for us to kind of like maybe give some questions to ask to the medical professionals to make sure all of our ducks are in the row, or any other tips for patients. I know we talked a lot about self advocacy. I just wanted to mention that, we know that it's so hard to do that. All of us having to manage our own care is one of the most exhausting things that we have to do and making sure doctors are communicating and doing their job should not be at the top of our list but it is because you have to make sure that you are, you are the one that's making sure all of the boxes are checked because you never, no one else is going to be able to do it better than, than you do when you're being able to reach out to all of the different specialists and things like that and unfortunately that's just how it rolls in our healthcare system that we do have to be our own self advocates and we also want to know that, want you all to know that it's not, we know that it's not easy. We say it all the time, but it truly is like one of the most frustrating things that even people who don't have our diseases go through also.
[00:50:00] Deb: Agreed. A couple things that come to my mind, again, I've had many surgeries is just plan ahead and give yourself grace after you have your surgery. You can't expect yourself to be preparing meals and doing laundry and picking up around the house. You've got to give yourself grace got to do that. Some of our best things that we've had is our church, people would take turns bringing us meals. So that was a good godsend. Otherwise, we would have starved because I wasn't cooking I do I do have in my freezer by backup meals for emergencies like our bad days. I, I do have my freezer stocked with some of that. So that's actually helpful but in my book is being as informed as possible and asking as many questions as you can think of. I know when I went in for my knee replacement, I wanted to know worst case scenario and what that looked like. My husband's like, why would you want to know that?
And I'm like, because if I wake up and that's my situation, I need to wrap my head around it. So some of those things, there are some things, talk to your support community like Kerry talked about. When I had my wrist fusion, this is my right hand, something they didn't tell me is that I wasn't going to be able to wipe my bottom, you know, after surgery so that became kind of a thing that I had to kind of figure out on my own and my left hand obviously doesn't work as well as my dominant hand so just try to think of is go in with lots and lots and lots of questions and throw things out there on social media and your, your people around you will support you and throw out some not great ideas but at least you're you're hearing different things that if you have a question you can add it to your list to take to your doctor. That would be kind of some of my summations.
[00:52:23] Kerry: Yeah, I would piggyback off that with just with some of the specific questions. Ask your doctor, really ask your doctor what you can expect. What you can expect in terms of, you know, what does recovery look like? And of course, to an extent, what they're going to say is it's really different for everybody. You want to have an idea. Ask them what kind of tools are you going to need? What kind of adaptive devices are going to help you if you can't wipe your bum? What, you know, because there are tools for everything. What are you going to be able to do? What are you not going to be able to do? Some things there's a specific timeline. For instance, I have, I'm still in my hip precautions, which means that I am not allowed, whether I physically can or not, I am not allowed to bend at the hip past the 90 degree angle. I am not allowed to turn on my side or cross my legs. And that is just a three month period.
And it doesn't matter how good I'm feeling or how bad I'm feeling. I am not allowed to do that. I have it in my calendar when I can finally sleep on my side. I cannot wait. But, you know, there are some things that are specific like that. There are other things in terms of the walking, in terms of when you might move from using a walker, a wheelchair, to a walker, to a cane, to on your own.
And a lot of that is just kind of based on how you feel. But you want to at least have an idea. Let them tell you you're going to start out with this adaptive device. And when you're ready for it, you'll move up to that. So
those are some of the specific questions of really, you know, you want to get as clear of a picture as possible of what your routine is going to look like and what you're going to need help with because there will be a lot of people who say, oh, let me know if you need anything. And while of course they mean, well, it's, that's one of the offers that just, I feel like that sort of puts the burden back on me to tell them what I need or to come up with something that they can do, but if you know ahead of time that you're not going to be able to cook, and somebody wants to offer to, you know, pick up dinner for you once or twice a week, that's awesome. But you need to have some idea of what those things are going to be. It might be that you are just going to need company. It might be just as equally valid of a want and a need and deserving of being met. You might just want to be left alone. And sometimes that's the best thing somebody can do for you is just give you that space.
And, and so that's, you know, the, the kind of thing, you know, asking your doctor, but also asking the arthritis community here, the AiArthritis
community, what kind of questions you should ask, what kind of things you should know, because that's where you're going to get a lot more of an idea of where you'll be, then just I'm going to get a hip and then I'm going to be walking and all right. There is a lot in between there. Yes.
[00:56:02] Leila: And if anybody who is going through a specific surgery wants to find other people that went through that same surgery or have any questions, you can email me at Leila@AiArthritis.Org and we can figure out a way to also maybe, you know, elevate your question, repost your posts and things like that. So we can have our patient community be able to help you, because, you know, not all of us are, are advocates or, or influencers where we have a big social media, kind of place where we can go to, or there's also Facebook groups and things like that, but you can look for I did something similar where, you know, with the younger generation, I searched it on TikTok and I just looked at my hashtag of a gastric sleeve surgery and always, you know, just went through, the TikToks to see the different stages that people were in and what they were eating at their different stages. And I think one of the biggest things was noticing that my surgeon, the, the instructions that they gave me were on the very conservative end and, I think that that is, something that I realized that I was okay, there's certain things that you can push the limits with if, if that's what you really need to, there's some things that you can, you know, make your own decision, decisions about, that's what we always say is that we are the experts in our body and in what we can handle and that was the biggest thing that made me empowered was knowing that, you know, yes, there's guidelines that you have to follow, but there's also, you know, power in knowing that you know your body best and if something doesn't seem right or something like, for example, the list of foods that they give you to eat right after surgery didn't have, you know, any of the Asian food that I usually eat.
So I had to specifically reach out to my dietician and ask her, can I eat ramen broth? Can I eat pho broth? Can I eat seaweed? You know, these
different things at what stage because the menu that they gave me, quite frankly, was catered to a Caucasian person. So, I had to ask all those questions myself and, you know, let them know, you know, I eat a lot of rice. If I want to eat rice, how much can I eat at this stage? And they're like, you know, just one scoop. I'm going to eat that one scoop because I want to eat my rice. So I just needed to make sure how much I needed to eat and things like that. So just taking it into your own hands and of course, following your, your surgeon or your doctor's guidelines as much as possible, but not to be afraid to push back and ask the questions that you feel are important.
[00:58:49] Kerry: And one other, just another really great resource that I will offer is if you, if you're going to have surgery or heck, even if you're not, and you're just dealing with AiArthritis, and challenges that it presents, Cheryl Crow, if you follow her on any and all social media, she is an occupational therapist and she also has autoimmune arthritis, AiArthritis, I think RA, I'm not 100% sure, but she has some form of AiArthritis, and so she has the knowledge coming both as a professional and as a patient, and so she really has, she has videos and, and webinars and all kinds of programs that she puts out giving all kinds of, lists of adaptive tools that you could use to help with a lot of the challenges that, that we might have. So she's a really great resource to check out.
[00:59:52] Leila: Absolutely. Cheryl Crow is a really, big a friend of the organization. She also has been on, the Arthritis Voices 360 show, I think once or twice. So she has been a guest, and we love promoting all of her, her things. She's very good at what she does and is an amazing tool and advocate for anybody who's looking for like those adaptive tools and things like that. So, I just wanted to give the floor if there's any other last minute things that we want to say to the listeners out there.
[01:00:26] Deb: I'll just add one after the fact because again, I, I have lots of tips because I've had lots of surgeries and I'll add some of those, when we launch the episode.
[01:00:38] Leila: Okay, sounds good. Well, thank you all for listening and thank you Deb and Kerry for being here. I really appreciate it and, I'm so excited to put out this episode to the public and again, if any of you have any questions, any comments, to anything in this episode, you can email us at info@AiArthritis.Org or you can, you can, personally email me at Leila@Aiarthritis.Org and I wanted to again, thank you all for being here and yes, AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www.AiArthritis.Org. Also, be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.
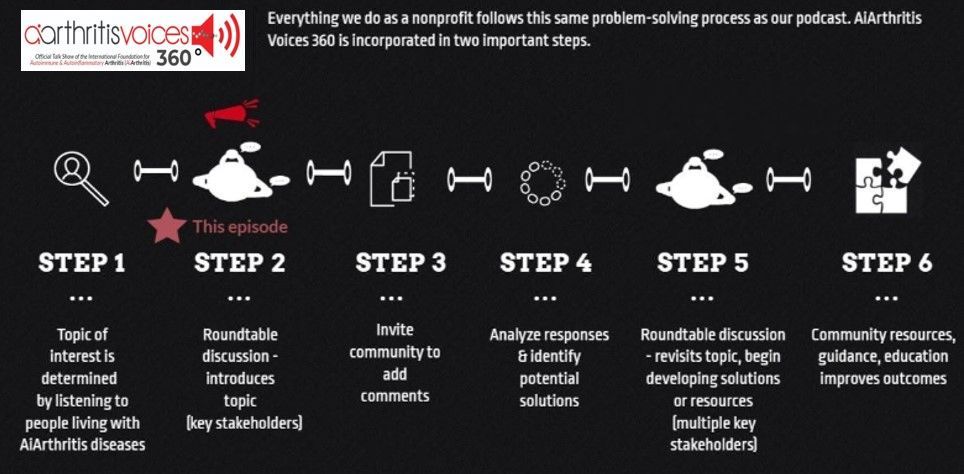
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!
-
Additional Resources & Information
Donate to Support the Show: https://www.aiarthritis.org/donate
Sign up for our Monthly AiArthritis Voices 360 Talk Show newsletter! HERE
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on Feedspot!

And now, let's 360it!
The main Sunday episode is where we "put the topic on the table," but it's not where the conversation ends! Now we spin off the conversation into different discussion segments. Below you will find several 360its. Some are videos from the main episode, while others are audiograms (soundbites).
Soon we will be launching additional 360its, which will build on these conversations. We'll hear from patients in the United States, Canada, and Australia who are here to help you through the transition to biosimilars. We are also planning a WATCH PARTY, where we will play back segments of webinars that aim to teach you more about biosimilars - and you'll have your fellow patients at AiArthritis to talk through it all with you! Stay tuned.
360its & SHORT VIDEO CLIPS FROM THE MAIN EPISODE
Managing Surgery Qualifications & Being Your own Advocate
In this episode, Leila and Deb share their experiences and preparations for surgery while managing AiArthritis diseases. Leila discusses her weight loss surgery journey, including the challenges of her high BMI and medication adjustments. Deb highlights the importance of self-advocacy and the need to assertively address health concerns with medical professionals. They emphasize the crucial role patients play in managing their care. Watch to gain insights into their remarkable journeys.
Your Host: Who is at the Table this Episode?
Leila Lagandaon
Leila
is the Health Education and Engagement Manager at the International Foundation for AiArthritis. She is a person living with Lupus Nephritis and Sjögren’s Disease. She is passionate about inclusion and diversity in health education and meeting individuals where they are at in order to learn in a way that resonates with them. Leila is on social media as @LupusLifestyle.Lei sharing bits and pieces about her life with lupus and connecting with others. Connect with her on Instagram or TikTok.
Deb Constien
Deb Constien
is a medically retired Registered Dietitian and a Representative for the AiArthritis with Rheumatoid Arthritis. Deb is also on the Advisory Council for WREN- Wisconsin Research Education Network and a Patient Family Advisor- PFA on an International PCORI research study for ACP- Advanced Care Planning.
Kerry Wong
Kerry
was eventually diagnosed with Fibromyalgia, Sarcoidosis, Small Fiber Neuropathy, Rheumatoid Arthritis, and Sjögren's Syndrome (to name a few). Kerry is a volunteer at New York State Advocacy Chair, Ambassador with Arthritis Foundation, and Patient Ambassador/Peer Mentor with Foundation for Sarcoidosis Research. Kerry does all she can to support the arthritis, sarcoidosis, chronic illness, and rare disease communities
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Mini-Episode #1: Mobility issues due to surgery, disability, or flares
Mobility is a key theme we will cover in many episodes. In this first mini "At the Table" episode, we are discussing situations that patients may face when normally able to put pressure on their foot/feet and then suddenly are challenged to walk (or anything else involving the feet). We featured a story in this episode from Deb, who has had foot surgery due to Rheumatoid Arthritis and is unable to put weight on it for up to 12 weeks.
Episode #18: The Juggling Act: Living with Multiple Conditions
In this episode of AiArthritis Voices , patient co-hosts Tiffany Westrich-Robertson and Simon Stones discuss the prevalence and logistics of living with multiple conditions.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.













