Breaking Research: Pharma & Non-Pharma 2023
AiArthritis Voices 360 Main, Full Episode 92
Air Date: December 3 , 2023
This episode is a Step 5, as outlined in our 6 Step Patient-Led Problem Solving Process.
Join us in this episode as co-hosts Tiffany and Deb both a recap of the 2023 ACR, American College of Rheumatology Conference and also how these topics specifically affect AiArthritis diseases. Tiffany and Deb also share an insight into our program, “Go With Us!” to Conferences. The Go With Us program allows patients to attend these conferences in real time and get updates on different important or emerging topics for AiArthritis diseases.
In this episode, the co-hosts discuss some main conference topics, both pharma and non-pharma, such as how precision medicine can greatly benefit patients by matching correct treatment plans, how existing treatments are being retested for subgroups and how lifestyle can impact your treatment. Learn common questions doctors receive from patients about their day to day life such as exercise, stress and diet and their advice on how lifestyle modifications can also help to alleviate symptoms. Don’t miss this patient recap of the 2023 ACR conference!
To join the Go With Us program, click here:
https://www.aiarthritis.org/conferences
To learn how to volunteer with AiArthritis, check out our program here: https://www.aiarthritis.org/volunteer
Come be apart of the AiArthritis Research Database here: https://www.aiarthritis.org/database
To learn more about JIA project, click here: www.aiarthritis.org/JIAcommunication
Episode Highlights:
- How lifestyle modifications such as exercise, stress and diet can help alleviate symptoms
- Understanding what parts of your immune system is being triggered by your disease for matching to the best treatments
- Discussion on how early should early intervention be done for JIA
- The importance of understanding precision medicine to improve matching the correct treatment plan for your AiArthritis disease.
- AiArthritis Go With Us program where you are able to attend the conferences such as ACR and EULAR in real time to understand current and emerging topics that relate to AiArthritis diseases.
- New therapy option in the very beginning stages being discussed at ACR that has the potential to suppress and protect from autoimmune arthritis diseases.
- Why supporting research is so important for the development of AiArthritis treatments
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient co-hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide to solve the problems that matter most.
Whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table.
[00:00:43] Tiffany: Welcome to AiArthritis Voices 360 this is the official talk show for the international foundation for auto immune and auto inflammatory arthritis or AiArthritis for short. My name is Tiffany Westridge-Robertson. I'm the CEO of the organization, original founder, and like all of the leaders at AiArthritis person living with our diseases, my primary diagnosis is non radiographic axial spondyloarthritis.
I'm like, I almost laugh every time I say that because it's so long and then a mix of other things. And as usually the way it is, as our talk shows, I'm not alone. I am here with longtime volunteer, Deb. Hey, Deb.
[00:01:32] Deb: Hey there. I am Deb Constien. I live in the Madison, Wisconsin area. Lots of snow on the ground right now.
And it's just the end of November. So that's a bit of a surprise. I was diagnosed with rheumatoid arthritis at the age of 13 and I've got a good handful of other comorbidities. So yeah, after 40 years of disease activity, it's gonna definitely take its toll.
[00:02:01] Tiffany: All right. Well, Okay, we got some exciting stuff to talk about today.
And for those of you who listen to our podcast in audio form, you can't see our screens, but if you're ever interested, you can go to our website and find this episode page and also go to our YouTube channel because we do record these on video as well. And if you're watching this on video, you see the screens behind Deb and I are both conference and that gives you a hint on what we're going to talk about today.
So hot off the press, our team just got back from the 2023 American College of Rheumatology or ACR Convergence, which is the biggest rheumatology research conference of the year. We go to that every year as well as to EULAR, which is the European Rheumatology Conference as well. So they're about every half a year we do this.
And with that, we have what we call go with us to conferences, which is my favorite program we have in our organization, probably because I lead the research department. So, that's why it's so exciting to me. And we have, not only are we broadcasting this as part of the go with us program so you can get a better idea of what that is like.
And so maybe you want to sign up for free to get updates and go with us when we do these, which is at AiArthritis.org/conferences. We're even going to tell you how we're going to expand this again. We keep expanding it and improving it. So stay tuned for that, because that's kind of exciting.
If this is something that you think might be of high interest to you to get more involved in, we will have a program for volunteers that will enable you to do that. So a little background, just go with us to conferences. What it is, we, Deb and I kind of started co creating this back in 2019 and the concept a derived because we would post on our social media about being at a conference.
Well, you know, years before this, we've been, I've been going since 2013 and patients would say, man, I wish I could go. And a lot of the reasons why they couldn't, there were really, they were kind of narrowed down to two. One is it's very physically and mentally demanding. And I mean, we're talking, you're up in the early, you're, you've got events afterwards, then on top of it, trying to understand what the sessions are saying, because these are not for patients.
These sessions are designed for rheumatologists and for researchers. So they're extremely high level. So that was one of the things, you know, and just, not being able to travel and really kind of, I guess, combining 1 and 2 is just really hard to understand and be able to then relay back what this means to the patient in your health care journey.
And that's sort of what makes our program unique as well. So, we don't just disseminate this research back as you'll see as you hear Deb and I talk about it. We relay it to you and encourage you to talk about, Whoa, this is how that directly relates to my treatment plan right now or my healthcare journey.
So it's a really unique experience and it's led by people living with the conditions. So Deb and I were joined by Leila, our health education manager who has lupus nephritis and Sjogren's. As well as Eileen Davidson, who has rheumatoid arthritis. You may also know her as chronic Eileen, and she is also one of our community awareness staff at AiArthritis and shout out to Anika, our international advocacy and policy director, who was not able to join us, who was supposed to join us but she was ill and she represents the undiagnosed mystery patients. So her mother and caregiver, her mother is a person who is that undifferentiated can't quite figure out in the immune family, what it is. So in saying that I'm going to just turn it over to Deb just for a second and just say, Deb, why don't you, in your own words, tell everybody why you enjoy being part of this, go with us experience.
[00:06:19] Deb: So I think that goes to my schooling. So I graduated college with a dietetics degree as well as a double major in biology. So science has always been kind of in my bucket, and I always I understand the information given, because becoming a dietitian, it's pretty intensive and high level as far as understanding everything and how it affects the body.
So, it just, I think my journey specifically, I, I wasn't a practicing dietitian long because of my disease and, became medically retired, but this has become a passion. It helps me understand going to the doctor's offices, I can understand what they're talking about. So I think that is actually so interesting.
And the fact that it is the latest and greatest information, I think that's also is, you know, part of the experience and it's also, bringing the information back to all of you that I really appreciate doing, I'm able to do it in layman's terms. So you guys understand why it's important to your disease process.
And again, our diseases are very complicated and it just, we feel that it just brings value and just part of the journey.
[00:07:47] Tiffany: So yeah, absolutely. So and saying that before we start giving you a little bit of there's just a snippet really of updates as a Deb word. I just took your word snippet. So we're going to go over a few of the sessions that we saw out of dozens that we saw and will continue as a group to watch and report back over the course of the year because we do have access to the recording.
But that is part of what this go with us program is. So we're giving you a brief look into the type of information that you can get by signing up. We do email you, send you shorter videos, behind the scenes photos, that type of stuff. And if you sign up officially for our program and you choose to, you also can get, if you're a patient, has to be a patient voice, we can't zap in researchers or you know, pharma companies or doctors that it is just for people with living with the conditions. We zap you into a private WhatsApp group where you actually get to go with us in real time to the conference. So, it is the coolest experience, I think, and that's what we've heard back from so many people who have gone and we also have people from other patient organizations who go and just go with us regularly because they're like kudos.
This is like the coolest behind the scenes real life experience that you could have going to a conference. So really proud of it and that's just an extra something that you get to actually talk to us in real time and then we keep it open for a couple weeks afterwards and then close it down anyway the things we're going to talk about today are precision medicine, which is everywhere. If you followed us, you know that we've been talking about this for several years. Precision medicine is really about being able to find unique molecular signatures in your bodily fluid so that could be blood where I'm going to talk a little bit about in your eye today on one that I saw with Sjogren's disease, and it can be urine, it can be tissue samples. So using your DNA, your molecular cellular level identification that makes you you, and then putting that together with thousands of others like you so it doesn't have to just be 1 person. We're talking about thousands and thousands of people who actually share these commonalities, which makes subgroups and that is falling under the and then we can either expedite diagnosis. So we eliminate that whole mystery patient that many of us have been in our lifetime or continue to be also can match patients to the treatments that will either work or won't work for them like that one still blows my mind and that is happening in the cancer space.
So, it's on its way. This isn't something that it's like, oh, this is a pipe dream. No, it's not. It's actually in the research phase right here, right now, and we're excited to report back some of those things. Now, will they happen tomorrow in the doctor's office? No, but they're getting there and you as a patient, as a person living with this disease is very exciting.
And it also, as I said, it can, it can also identify if you would react negatively or have bad side effects. So, and, we're talking about prevention and some other things too, that knowing what these biomarkers are, knowing what these pieces are in your DNA and your makeup, if there's potential to know in the future, if you have these, could you actually prevent the onset?
I mean, mind blowing stuff. So we're going to touch a little bit on that today. We're also going to just talk in general about some of the existing treatments out there that are being retested for subgroups. Deb's going to talk about lifestyle, non pharma stuff, which I know is exciting to a lot of people.
And yes, It is at the conference, not just pharma and not just biologics, but it is also about diet and exercise they do about and I'm going to briefly just throw on the table and you'll have to tune into what we call a 360it. So this talk show being AiArthritis voices 360 means we put the topics on the table that and some of these we won't branch out until after the fact into a breakout video 10 minute type of thing.
And that is dental care. So there were like 3 or 4 sessions on just dental care and how it is starting to be recommended that rheumatologists mention this during a visit and become part of a regular treatment plan protocol and interdisciplinary care, if you will, when all of your specialists work together because it's, because I just had a cat run across my lap. I saw that if you were on video, maybe and so I'll just touch on that again towards the end, but that will be a breakout conversation. So without further ado, I am going to turn this over to Deb and she's going to give us an update on what she learned about lifestyle management at the rheumatology conference.
[00:12:59] Deb: Awesome. So this particular person is a rheumatologist. Her name was Sarah Patterson, and she is from the University of California, San Francisco, and she's part of integrative health. Integrative health is other things besides medication that can actually help your disease process. So the session was called leveraging lifestyle medicine to improve the quality of life in rheumatic diseases and the specific diseases because the research is very limited in this area. So they aren't very big studies. So they tend to be maybe 12, 15, 25 people that took part in these, the research. So she is actually talking about the limitations of some of the research and the two diseases that there is the most research on are rheumatoid arthritis and lupus. So those are the two diseases that are specifically commented on in this session.
So the one thing she opened up with was common questions that she as a rheumatologist hears from her patients. So the first one, are there ways I can change my diet to help my disease? Can I exercise or is exercise bad for my joints? And how does stress contribute to my disease? And are there ways that I can reduce stress without medications? So those are really powerful questions that I'm sure, Tiffany, you would probably nod your head that people are asking all the time.
[00:14:48] Tiffany: Oh, yeah, for sure. And, you know, just a side note, one of the projects that we're working on at AiArthritis and juvenile arthritis for these communication aids that help the conversations moving in all phases of the diagnostic and therapy journey.
And while those questions are very relevant in the adult population, it has a whole different dynamic in the family dynamic because think about that. It's a well, you know, Deb, you were diagnosed at 13, the decisions that we make as adults are our decisions, but the parents are having to make these decisions and they're fearful often about biologic treatment, early intervention, and it's not uncommon that they're asking about lifestyle, diet, exercise, what is the potential of doing that first? You hear that a lot because I mean, they, they are really trying to understand this. So it's just, I just wanted to throw it out there it's a different dynamic, but this is something that a lot of people ask. There's no doubt.
[00:15:50] Deb: And it's funny, you should say that again, I do all the specialty diets at the camp that we have here in Wisconsin, and there are typically about 90 kids that go to the camp and a couple of years back.
It diet exploded and they're typically parent imposed diets that are limiting whether it's gluten free, dairy free, soy free all these different modifications to the diet and I regulate all those and the kids come to me for the different choices that I offer and I make them fun too because as a kid you don't want to be looked at differently. So it definitely has gone through the ups and downs right now. I think last year we had about 15 kids, but at the highest point, there were about 30 out of those 90 kids that had specialty diets and restrictions. So I get it. That would be the first line of attack that I, as a parent would want to do, I guess, to as a kid, you know, for my kid, instead of putting them on some scary looking meds, but
[00:17:03] Tiffany: yeah, but although we know that early intervention is also important. So I will swing back. I wrote myself a note here. I didn't we didn't we just do this. We didn't mean to segue, but it made me remember the debate this year was to treat or not to treat early in JIA. So I'm going to segue that after you're done, Deb, into what I'm going to talk about next.
[00:17:27] Deb: Awesome. So getting back to this session. So she broke this down into, you know, four different lifestyle modifications. The first one being a healthy diet. Second one being physical activity. Next one stress resilience, so stress reduction and other lifestyle factors being in there. So that was a separate little bucket.
So I'm not going to go into tons, but I want to get down to the crux of what she talked about is she went into several different studies, a lot of them only being very little information and very few people that actually participated, but there ended up being 3 different things. So dietary interventions for RA was actually discussed diet and disease outcomes with lupus and Omega 3 supplementation.
So, Omega 3 fatty acids are something that you tend to find in fish and things like that. So, those are what the fatty acids are in food. So. Basically what it came down to and she really got into a lot of the information that the take home information was the plant based whole food Mediterranean diet.
So the Mediterranean diet being vegetables, fruits, olive oils, whole grains, beans, legumes, legumes are different kinds of peas and things like that fish, low fat dairy, lean poultry, nuts, and it limits red meats and added sugar and processed foods. So the sweets and the things that like hot dogs and lunch meats and things like that.
So that's kind of what the Mediterranean diet is. What more plant based is eliminating more of the red meats because of heart health. That's what it kind of comes down to. So it came down to how this actually just affected the patients and they found that they, they have something called the DOS. It's the disease activity.
What is that asked? Disease activity.
[00:19:57] Tiffany: Sorry, I was on mute. Disease activity score.
[00:20:00] Deb: Score. Thank you. So, it's the joint counts. How many swollen and painful joints you have. They found that when that diet was used, it reduced pain and it also reduced the disease activity and rheumatoid arthritis. Patients with lupus experienced improved in symptoms after adding that specific diet, the plant based with Mediterranean diet.
And it says that we still need to do larger sample sizes in the clinical trials that there are out there because they were, they were based on like nine people or six people. So to actually get a bigger study out there so you can actually tie the actual diet to that a little bit better and that fish oils.
So fish, there's a supplement you can buy. It's called fish oil. It's a supplement and it said that using that definitely improves the disease activity in RA and lupus. So adding a supplement, they were adding let me see, what was the amount of the supplement? The omega 3 and omega 6 polyunsaturated fatty acids.
So that's what that capsule is made up of, of those two in particular that are more heart healthy. So it does improve the disease activity in your body and you're not having as many sore joints. So that in a nutshell was based on the diet as far as
[00:21:40] Tiffany: let me ask you this, Deb, do you take fish oil every day?
[00:21:43] Deb: I used to, but I found that when I would, cause it's like 3 or 4 of the capsules and I found that I was burping and I didn't like that.
[00:21:55] Tiffany: Side effect.
[00:21:57] Deb: Yes, and it's kind of my own. There's people that have no problems doing it.
[00:22:02] Tiffany: I take it every day.
[00:22:03] Deb: Do you? Okay.
[00:22:05] Tiffany: Yeah.
[00:22:05] Deb: And do you have anything like that? That
[00:22:08] Tiffany: not that I, not that I know of.
Not that I, the only thing is I, I, I know that it is like a blood thinner. And so when I have to, there's, I, yeah, I'm a bleeder and I always asked, are you on fish oil? Because if I'm stuck or what, you know, I bleed like crazy. So that's the only side effect. And I'm, I don't plan on bleeding or being cut off
Yes. So it's not something that deters me, I, I don't know how much it. I mean, I'm glad to hear that it can improve heart health, but, you know, that's, I was actually, I take it because of joint pain. I don't know how much it helps. I can say that I would never use it without other, like, in addition, I would never substitute for, you know, there's no way.
I don't have mild Yeah, Very mild disease, but that's very rare actually to have very mild disease. So, I definitely wouldn't use it as a sole treatment, but I do incorporate it daily.
[00:23:10] Deb: Yeah, and I, like I said, I used to, but my I'm doing I'm choosing not to because of that specific reason I literally would burp oil and Yeah, and it would yeah, so okay.
It just wasn't a pleasant side effect for me So I kind of knocked it out. So the next piece was on physical activity. The first study that they actually looked at was physical activity, is it important for the patient reported outcomes in RA? So it was looking at it in RA. And the first question that was asked is, is physical activity safe? And there are a lot of people that in, I, I think I was in that bucket once upon a time before I became more educated about it that, you know, you always hear that phrase of motion is lotion and it is kind of like that with our, with our joints. So they definitely said in many studies, and whether it's even just walking, that physical activity is in keeping your joints moving is very beneficial to RA in particular in this study. The other piece that I found very interesting as they did bring up the 2022 American College of Rheumatology guidelines for rehabilitation, diet, exercise, and additional integrative interventions for rheumatoid arthritis. And myself and Eileen were listed on helping out with that project. And the one thing that they did, out of all of the recommendations out there, the one that was a strong recommendation and not conditional recommendation was they strongly agreed that regular, and this is patients and rheumatologists that created these guidelines. It was the only one that was strongly recommended was for exercise.
So that just stood out to me and just how much this actually helps. They did talk about high intensity interval training. So again, depends on the patient and the level of exercise you choose. So you need to specifically talk to your rheumatologist or have them send you to a physical therapist so they can individually determine what is appropriate for you.
Because something might if you're doing repetitive motion. I know that I had a job where I was cutting material at Joanne fabrics and that repetitive scissor motion caused my shoulder to flare. So, yeah, not a good thing. So they talked about physical activity and fatigue in particular
[00:26:11] Tiffany: just gonna say I when you were because I was like, well, joints, that's Fine.
But as we all know, these diseases, that's only one component of our diseases is the joint. So I'm sitting here thinking to myself, I try to go back to go to the gym, working out at home just isn't, I don't know. I can't get motivated. I really do have to be in a gym for my own motivation, what I have you, but the fatigue is what gets me.
And if I'm flaring, it's not necessarily my joints, it's my tissues. And I have spondyloarthritis, which means emphysitis. So that's the connective, that's like the tissue that's connecting your bone, right? And so it's a different feeling than the joint pain. And that's what holds me back. And so it's not that it's, I know it's good for me, but the thought of even trying to do that when I'm in pain or when I'm super fatigued that's what dominates my exercise regimen more than anything.
[00:27:07] Deb: Yeah to like, think about having to go someplace to do something my motivation like stops me flat because my fatigue is bad all the time.
[00:27:17] Tiffany: And it's not like the thing with our fatigue is it's inflammation driven. And so my, I guess my question and I don't know if maybe they did cover this because you mentioned fatigue. I don't know. Deb and I did not pre prep for this. I have no idea what you're going to say, but like for me, I feel like if I'm flaring, it's not a good time to exercise because if I'm already feeling like this and I overdo it, I feel like it's going to make me worse.
And that's just like the same thing like if I'm doing laundry or if I'm doing the dishes or I'm trying to do stuff around the house, I know if I'm already in that state that I'm just gonna get myself worse. So anyway, that's what I'm thinking about with exercises. It's not like with OA with osteoarthritis where, you know, jump in a pool and sometimes that's going to help yourself out because it's a, it's more of a mechanical type of pain.
Whereas this, yeah, it does feel worse when you sit around because it's stiff, but at the same time the thought of going to the gym and being on a treadmill or something like that, I just can't if I'm flaring.
[00:28:21] Deb: I get it. Yeah, I 100 percent get it. This one study was looking at physical activity effects on lupus and it talked about that they definitely saw it reduces the severity of fatigue and lupus.
And there were 5 different studies that it talked about that specifically, it also talked about just improves the health related quality of life. So, if your quality of life, if you're not able to participate in life and go to friends. If you're like saying that you're don't want to go out for dinner with your friends and you don't want to go do this and you don't want to go to do that, that affects your quality of life overall.
So they did talk about that too and it was just very interesting to see how much exercise and inflammation they were talking about how much it lowers the inflammation markers in your blood by actually moving. And again, it can be something as simple as walking, because many of these studies were about just dedicated walking for X amount of minutes and increasing that over time.
So definitely interesting as far as that went. And they were talking about the take home points. So basically physical activity. They said that physical activity reduces fatigue, improves quality of life, and improves sleep. So your sleep interruption in RA and lupus. They said that the patients that were rheumatoid arthritis and lupus patients who were more physically acted had also been able to deal with down regulation of their innate and adaptive immune signals and genes, so it is how your body is reacting and that physical exercise and activity definitely has a positive influence on your immune system.
[00:30:35] Tiffany: So Deb said the adaptive in the immune system. So I'm going to tell you this is what this is what we do here. This is what one of the things that makes our debriefs very different. We're not just reporting back what we learned. We're talking about how these words, how these things actually mean something to us in our diseases.
So in saying that, AiArthritis we represent people with autoimmune and autoinflammatory that part that autoinflammatory disease tends to get knocked off for some reason, but there is such a thing and basically you have sides of your immune system. You have components of your immune system. The innate is what you're born with, and that is traditionally thought of as an autoinflammatory disease.
They tend to be rare. They tend to have younger onset. And then you have the autoimmune, which is the adaptive, and it's right in the name. Your immune system, there's something that has to happen, some environmental trigger that your body is learning a response to and reacting to a response to where it attacks your own immune system, thinking it's an invader.
So it's adapting to something. It has to have a learned response, and there has to be an environmental trigger. Whereas innate is innate it's in board there does not need to be in it, but it can have an environmental trigger, but it does not have to and saying that I think it was around 2016 was the 1st time I had heard and I believe it was at the EULAR conference in a lupus session where they put on the table this idea, this concept of the immune systems overlap, and now they're starting to see that both sides can be triggered. So if you have lupus or RA, which are traditional autoimmune or adaptive side of your immune system triggered, that it can trigger the cells and the molecular structure that is more common in the innate part of the immune system, which I think makes total sense.
It's your own immune system. I mean, if inflammation is running rampant, I don't see why it wouldn't cross over in some way, shape or form. And that could also be why we think That these diseases are so alike, regardless of what side of the immune system, they probably all have a little bit of a crossover here and there.
So, I just wanted to take that opportunity to do a little breakout to explain what that meant, because that is relevant for all just to understand your disease. And that also matters when we're talking about treatments, as we'll go into here next, we're talking about matching to the right ones.
Understanding what parts of your immune system are being triggered is going to be important for matching you to treatments that are going to be working best for you. So
that makes perfect sense.
[00:33:22] Deb: And I appreciate that because my brain was not, I wasn't triggering on the definitions at that moment, so I appreciate you stepping in and saying that
[00:33:33] Tiffany: No problem
[00:33:33] Deb: Awesome. So the next. Okay. So that is kind of the summary on exercise. So exercise is good. The next piece was stress. So it's funny. They were talking about what stresses as far as the definition goes. So is it stress like an exposure or an event, something that puts stress on your body? Is it your perception of how you're thinking about it?
Or is it your flight? A flight or is it freight and flight or something like that? So basically, you've gotten scared. So what are you going to do? You're going to run away. So that imposes stress on your body as well. But for this session, she was talking about the psychological stress that when a person perceives and in the environmental demand that is exceeds the adaptive capacity. So exactly what you were just talking about. So how you are perceiving a stressful moment. So it takes all of those things, whether it's an event or how you're perceiving it, it takes all of that into into accounts when so that's the kind of stress that we're talking about in this particular instance. And it talks about different mechanisms that were put on to you.
So they basically went into a couple different studies that talked about how the mechanisms that affected affect your stress on your physical health, because how you perceive the stress is going to affect you so it could actually cause depression. There's a lot of people that get stuck in that cycle of the woe is me and I get it.
I have my bad days too. So I do understand that they talk about chronic stress can provoke an unhealthy lifestyle practices. So bad sleep, inactivity, smoking, or other substance abuse, and it also will affect your immune system overall. So, it can also cause a greater risk of depression. So, you're having less pain tolerance.
You're having increased increased fatigue and your worst perception of how you feel your health is. So you think everything's in the toilet. So your overall health is just terrible. So they talked about some different things that are stress interventions, whether it be mindfulness, which is actually thinking about it is being aware of every part of your body. You can use mindfulness as it is. You can use yoga, tai chi, biofeedback. There's a lot of different things that you can do as far as some of the interventions. I actually took a mindfulness class that was 16 weeks and they are like three to four hours each week that you're in this and it's practiced every day.
I found it a little overwhelming. I did see the benefits of it, but it's a lot. So, you can go into a, like lay in bed and you close your eyes and you're thinking about, okay, so feel your fingertips, feel your hand, feel your wrists and you go through every single part of your body. So it is super beneficial for a lot of people.
They found that using a mindfulness intervention, that it affects patients with chronic pain, the, it reduces the pain intensity. And it decreases the chance of anxiety, and it decreases depression, and it can improve your quality of life, your physical function, and your sleep. So actually having better sleep outcomes, which It, Again, everybody wants to achieve those things, so that's pretty much it.
There was some more information, but basically, um, it came down to the conclusions of this entire session was that the plant based whole food Mediterranean diet reduces pain with RA. The physical activity improves patient reported outcomes in RA and in lupus, it talks about better quality of life, physical function, the less pain, and your better quality of sleep.
And let's see, high reported stress predicts worse clinical outcomes for both diseases, lupus and RA, and that mindfulness based interventions improve symptoms that are prevalent in rheumatic diseases, so it covers the gap. And the things that she talked about, potential for future directions of these type of studies, Is having larger clinical trials, more people that are involved with different rheumatic diseases .That the physical activity in RA and lupus to establish more effective activities that are able to lead to positive outcomes.
And yeah, that is pretty much it. And then she credits a lot of different base, like she has a lot of, they, she and another dietitian created a database and that any patient can go to, and we can actually add that maybe as an attachment at the end. Yes. Yes. It's on their website that they created.
[00:39:51] Tiffany: Okay. We will, we will add that. All right. Okay, so okay, well, that was awesome. Thank you so much. It's such a big thing that people want to know. And I just think it's important to understand when we go to these conferences. It's not all about biologics and pharmaceutical it, there's a lot going on in research and so we did the end of the 1st half for non pharma. And then we're going to do the second half for the treatments and really focusing on this precision medicine, which I mentioned earlier is about understanding your own individual signatures and how would you group those with thousands of people? We're creating subgroups and I'm going to give you some examples of what's going on in precision medicine in our space.
And saying that for those who had tuned in a little bit earlier, we were talking about juvenile arthritis and one of the the debate they always have a debate and the big debate this year was how early do you intervene in juvenile arthritis? And so just quickly there was there wasn't like a winner of the debate.
Usually there's like a winner and it was kind of just torn in half. I mean, it's, it's really, I think, about shared decision making with the doctor and the family. There's a lot to consider, especially because juveniles are not, do not have clinical trials that often. There are some of the biologics that there were clinical trials.
And they are indicated for juvenile arthritis, but a lot of times it's just borrowed from the adult versions and that, you know, that does make it a little bit of a scarier situation. And there's a lot of questions around growth and, you know, they're just a lot of questions. And so the bottom line was, we know there's data that shows that early intervention and our diseases gives us the best opportunity for remission, but in the lack of clinical trial research in people in juveniles, there are still questions on what how early is early. How early do you start in a child versus an adult? And there was no answer, but I just wanted you to know that it is something that is being talked about and discussed. So I thought I would throw that out there because it was a good, it's a good transition to and to just talking about treatment. So what I'm going to do is. There were, I mean, there are thousands of sessions and summary posters, which are called abstracts at these conventions. So there's no way we can possibly cover everything, but the good news is I mentioned in the beginning, we have this go with us to conferences program, and that's where we're doing exactly what we're doing now. We're looking at information. We're reporting back and we do have access to these recorded sessions and all of these summary posters or abstracts all the way through October of 2024. Well, abstracts really forever, but we have the recordings of the sessions for a year. And that's just part of purchasing that passes for the conference.
And so we can continue to go back and report for you, which is why it's awesome to sign up for this program. Because just because the go with us experience ends, it doesn't mean that the data that we collect to report back has to end. In saying that also, we have this new addition, if you want to be a volunteer with arthritis, this is all very exciting to you.
You're like, man, I kind of want to see if I take a stab at watching some of these and seeing if I can report back. It does take skill. I'm not, I'm not going to lie. This Deb and I couldn't do this overnight. This is years of going and kind of drowning out what I call the noise because these are directed at rheumatologists and researchers, not at patients.
And especially at the ACR at you are, it's a little different. They do have a patient track, but it does make it a little complex. But we are opening for the volunteer opportunity to do this with us. So if that is of interest to you at all, if this is like, wow, I would like to be able to learn how to do this.
You can go to AiArthritis.org/volunteer. So I wanted to throw that out there. All right. So one of the things that's happening is repurposing our treatment. So there's a lot of biologics out there right now. And I was surprised at first to see like Otezla, for example, this is one that that was pulled up and Otezla for psoriatic arthritis.
And I was like, Otezla has been for psoriatic arthritis for as long as I've known. So that kind of threw me off and it attracted me to the session. And so I thought, well, what are they doing that's different? And the things that they're really looking at is now that they're, they're starting to recommend the use of ultrasound. So we went from x ray to MRI to ultrasound is something we started hearing a few years ago. Let's be honest, not everybody's insurance or health government or wherever you live in the world is going to cover an ultrasound. And there are some remote places in the world that's not even an option.
So let's, you know, like, so, so in the sense of reality, I don't know how realistic it is. But we do know that being able to ultrasound your hands or ultrasound places of high inflammation can help redirect treatment. So that is just something to take away from this. So this was talking about ultrasound use and being able to do clinical trials using that method instead of what used to be an MRI, right?
So they're trying to show basically proof of concept that inflammation can be better detected, you can manage your disease better with ultrasound. In saying that it did show that there was significant improvement in inflammation after 6 months, but the drug was mostly affected for patients with moderate disease, but not with severe disease.
I thought that was very interesting. At almost a year, there was very little report of any structural damage in those with moderate disease. The reason I bring that up specifically is when I talked about precision medicine. It's about subgroups. Yes, it is about the individual, but I want you all to think about it more of thousands who are alike, because that is how you're going to gain access to treatment.
Nobody is going to go. It would be no insurance company, no government there is ever going to say, oh, I will give you and only you access to this treatment because it seems that you may respond to this. There's no way. And the reason why is because the healthcare systems are set up to be able to treat the general population.
And that's where this kind of back and forth conundrum happens because our diseases are heterogeneous, meaning they do tend to be unique in the onset and, and how they present in our bodies and how we continue forth with the disease itself. But, if governments, healthcare systems, insurance companies, all these can see data that show thousands of us, in this case, those with psoriatic arthritis who are classified as moderate, not severe, not mild.
There are actually those categories, believe it or not. And then, it might make more sense, there's an argument for the health insurance company, or the government that says you cannot use this drug because it's not on our preferred list or whatever you call it in your area of the world, because this one saves us most money and that's that's fine. They're supposed to save money. They have a lot of the pie to distribute, but if the data is going to show that, hey, I meet this criteria that is justification, perhaps, for overriding that decision and proving that I might benefit better, in essence, I won't have as many hospital visits or specialists or comorbidities or all these things that happen, and that saves money, not just for the patient, but for the health care system.
The reason I bring that up. If you are interested in doing, be participating, not necessarily these big clinical trials, but research with your fellow patients like AiArthritis. We have just started the AiArthritis Research Database, which is strongly going to be to talk to all of you, talk to your peers, where we're partnering, it's under Forward National Data Bank for Rheumatic Diseases and their servers.
They've been around for decades and so the research that we're conducting will be in survey form, but also talking to each other. We want to understand how you're responding to these so we can get some data to then turn around and influence public policy or legislation, which is essentially access to our treatment.
So if you're interested in that, it's AiArthritis.org/database , AiArthritis.org/database. So, these are the kind of things, non official clinical trials, but still real world evidence is what it's called, that you can be part of. So, if clinical trials freak you out, come on over to us, because we're, we're, we're not doing clinical trials, we're, but we are going to make sure that your voice counts.
So that was just an, an interesting one that I thought, and then just a, just a quick fact check when we talk about ultrasound versus MRI versus x ray. For those who do not know, if you are going through a diagnostic journey, x rays will not show our damage, our inflammation will not show inflammation only shows bone damage, right?
So it's our inflammation, the pain you feel start when inflammation before it ever causes damage. It takes years. Sometimes with aggressive disease, not as many years, but the average is 10 years from onset to show on an x ray. So don't be discouraged if your primary care physician or somebody orders all of these x rays and they come back, well, we don't see anything.
You're not supposed to see anything. And that's why they're pushing for ultrasound even more than MRI. And don't stop pushing if somebody says, well, I don't see anything on your x ray and there's nothing wrong with you. Wanted to make sure that people know that.
[00:50:12] Deb: That is actually amazing. My son had cellulitis at one point and it was ultrasound that was able to show the tissue damage with all of the inflammation.
It just, again, to most of us who aren't trained to look at ultrasounds, it looks like different shades of gray. But to the trained eye, it speaks volumes and is even more information than a MRI sometimes, as far as that specific part. Yeah.
[00:50:43] Tiffany: But again, I mean, who knows what, I mean, that's, that's adding to the unaffordability, but I really hope by adding the layer of ultrasound proof, it starts to just make the x ray fall off. Unless it's osteoarthritis that's a whole different ball game. That's going to show osteoarthritis damage and it also can show a years of inflammation damage. But unless you get into the point where it's affecting something that would show up on an x ray, it's not going to show up on an x ray.
So that's just something important to note. All right. So. I'm going to go quickly through this next, just in lieu of time here, knowing that we are going to 360it out meaning the things that you're hearing are just a little bit of all of the things that we've learned. And you can tune in to these break off conversations that will happen little bite size.
So it's not going to be another hour long. It will be 10 minutes at the max of each individual session or review, so they'll be very digestible and make sure you could find all of the 360its that we do from this episode on our website at AiArthritis.org/talkshow and then you just find this episode.
And you'll be able to, as we do the 360its they'll be listed on there. Okay, so precision medicine, I mentioned it, I don't know how many times, but essentially what I wrote on here, B cells, T cells, DNA, I mean, it's, it's all, you know, there are, we hear these a lot and that's why you hear like different inhibitors.
Our biologics will inhibit a T cell or it will inhibit a B cell or because those are the things that are overactive in your disease or presumed in your disease. And so there's a lot of these, but there's more that have been coming out. I heard of the importance of key selectin. I didn't know what that was, but the, the point, and you don't need to know exactly what it is either.
You don't need to define all of these. The point is that they're exploring other molecular structures so there is an advancement in our treatments. That's what we as patients want to take away, right? We don't need to know what all of these acronyms necessarily lead to. But there are, it says there's expanding evidence demonstrating the increased levels of those molecules and it's those are associated with a wide variety of inflammatory diseases, including RA Scleroderma or scleritis, lupus, spondyloarthritis, psoriatic arthritis, and interstitial lung disease, which is a comorbidity of our diseases.
So that's just a handful right there of this new molecular target, so that was exciting in itself that they're looking and expanding. I did a brief biomarkers search and I've already mentioned some of them, but also sarcoidosis, Sjogren's, Stills disease, lupus nephritis, which is when the lupus affects your kidneys.
And, and cardiovascular, which Deb has done some breakouts on that already. And we'll do some 360its for you on lot on cardiovascular risk. So they're really starting to go in on a granular level and try to identify these things early. And so in addition to early treatment, we're really going into this whole idea of prevention also.
One of the breakout ones, I just wanted to, just to give you an example of some of these studies. There was one on Sjogren's disease. There's a lot actually happening in show grants. And if you don't know, as of timestamp 2023, end of 2023, there is not, there are not any specific biologics for Sjogrens, it's a borrowed treatment disease. So that you're seeing a lot of research and we heard through our meetings there's, everybody seems it's the new hot disease and every there's always, it goes, it ebbs and flows. There's always a hot disease. And for a couple of years, it was my disease, non radiographic nr-axSpA, lupus is still really hot, RA always is because it's one of the easier to study, but Sjogren's is really moving up in this. So this was a study that talked about collecting biomarker samples out of a thin layer of tissue in your eyeball. Now, I have no idea because I didn't see any patient reports, like what does that feel like or anything?
But by doing this, the researchers were able to use a gene analysis called conjunct. Oh, God, I want to say conjunctiva conjunctivitis, but it's not conjunctivitis because that's it, but but conjunctiva imprints is what it's called and I'm sorry if I butchered that it's a, they say it's a powerful tool for understanding how mild or severe Sjogren's disease may be, and they can use this to develop new treatments that are targeting these specific genes that it's just another example of how to be able to start understanding your subgroup, mild, moderate, severe, and your potential response to treatments. That's what, that's what precision medicine is all about. So then another, I want to, another thing that they're talking about, this is, I wrote in my notes, early, early, early.
So that's when we say basic science or we see basic science in our description of the sessions that means mouse level that and so so when you think of, like, the very beginning of scientists and we're in the laboratory where they're using mice models to figure out if something can then move on to the human trials that is early. And it's a highly sophisticated and so I didn't go to the session for the sole fact that basic science is very difficult to understand, but somebody thankfully did a little short review on it. So I cheated a little bit and I went and looked at what they had to say and saying that it's called antigen specific preventive therapy.
And this is emerged after CoVid. So the session or that it was called a new therapy option and antigen specific preventive therapy for autoimmune disease and it is targeting antigen specific T cells and think of it as a vaccine. Oh, it says. A peptide used vaccine against autoimmune arthritis. That's the name of the abstract and it said the mouse models, so, again, basic science are showing that by precisely targeting these T cells with an approach, thinking of a vaccine, they are starting to see that it's possible to suppress and protect a person from developing autoimmune arthritis. That was just exciting. So just know when we say basic science to this is so early.
We're talking 10, 15 years before we see something like this likely in, in our, in our clinical space. So don't be like, oh, my God, there's gonna be a vaccine and we're all going to be, you know, cured or prevented. But know, this is exciting. Because this is actually something that's showing there's a potential for this.
I mean, something good came out of COVID, right? So that was really exciting. The new word that kept coming up, I saw it again, protective. So I wrote, we have a glossary that goes along with our Go With Us program. And every time we come up, we see a new word. And obviously, protective isn't a new invented word, but it's the first time I've seen it in any of the sessions.
Right, and so that kept coming up again, and it happened in some studies with lupus. In particular, so that is just super exciting. The other one that I want to throw out as an exciting and this is the last one and we'll wrap it up here is therapy updates. You may have heard of CAR-T, CAR-T therapy. I know I've seen it kind of thrown around in magazines and things over the years.
It's something that has been used in cancer for some time, and this, it's essentially a process that takes your own personal cells and feeds and feeds them back into you and uses your own cells as your treatment. So this is something that is being explored in lupus and other diseases. It says here, the one nugget that I took from this was in a study.
Now, this is only 15 patients and Deb talked about how, you know, the numbers matter, but also I want to point out that CAR-T in addition to cancer has been shown in rare diseases. So in this case the impact, it doesn't matter so much that it was only 15. So let me tell you what happened. So they did this CAR-T in a, in a study for short term efficacy of this therapy, meaning it's new.
They can't say this is forever because they don't know. All right. So that's what short term means in this case. Therapy and autoimmune diseases, 15 patients, 8 patients of the 15 complete remission and a disease activity score of zero. All eight patients discontinued their biologics after one infusion of CAR-T cell.
[01:00:21] Deb: Okay. You just saw me. I was like, that is amazing. Again, over 50%. .
[01:00:32] Tiffany: Yeah, completely. It's like 100, 0, 0 disease activity. No, painful. Yeah, no, nothing. Painful joints. Yeah. I mean, you can't use the word cure, but it's like complete remission now and again. The thing about to understand this is it's too early to know.
Does that mean you'd be in remission for a year? Does it mean five years? Does it mean 10 years? Does it mean forever? We don't know.
[01:00:58] Deb: Because they're just starting it, just starting it,
[01:01:01] Tiffany: But they're studying. I had to end this with mentioning that because there is hope out there. That's why we need to support research.
That's why this kind of information is so valuable. Will this happen in our lifetime? I hope so. If it's, if it's in the studies right now, that tells me where maybe a decade out or so, you know, so anyway, that's just really hopeful and exciting and a different way of treating other than biologics. It's using your own cells, repurposing them, putting them back into your body and basically self healing.
[01:01:41] Deb: That's amazing. So that was my mind. Yeah. In an exciting way.
[01:01:46] Tiffany: Yeah. So, in saying that, as you can tell, we've learned a whole lot, and we could talk for hours and hours and hours about this, but we've got to keep the episode at least at this hour at the max, which is where we're at and we wanted to, in actually a few minutes over, but, we do have all of this on YouTube as well, that is chaptered into bite size.
So if you wanted to go back and relisten or share with anybody like, wow, this segment in particular, you can do that. So you can just go to the YouTube, our YouTube channel, IFAiarthritis is the same on all of the social medias, and we have a whole playlist for talk show. So you can look up this episode beyond to be able to quickly share and then don't forget we have the 360its so we're not done. There's a lot of information that we've learned and we're going to keep reporting back. We have this new exciting go with us extension that in addition to you just signing up, you get these emails when we go to the conferences, you have the option of an elevated experience.
If you're a person living with the diseases to be in the WhatsApp group and actually be communicating with the people at the conference in real time, which is super cool. If you want to be a volunteer that must be a volunteer and you do not have to be a patient to be a volunteer with arthritis, by the way, we do have another extension of this that we're starting.
For our volunteers interested in research, where we will give you some access to our conference materials, and you can listen to these sessions. We can you can try to report back or at least take notes if you're not comfortable reporting back. That's okay. As we said, this is it takes a lot to get through the noise to get to those kind of nuggets to report back, but it's a cool opportunity to really learn and if there's something that's a passion or interest to you that that would be exciting for you and you would be helping us by getting more of this information back to our community, and we really do use all of the information we learn in the projects that we do. So there's a lot of ways that your contribution can impact millions of lives around the world because we take these, these nuggets of information and we're able to create resources and improve communications with doctors and, and improve your health care journeys as well.
So, in saying that Deb, thank you so much for
[01:04:13] Deb: pleasure. I just really enjoy this. And again, we don't know it all either. And we do look it up and that is the best way of learning how to do all this. And if you choose to do this too. You can keep replaying back like, what did they just say? And you can listen to it 10 times.
Yeah, it gets into you and that is, that's almost a better way of doing it versus the in person because you only hear it once. Yeah,
[01:04:42] Tiffany: true. That's actually a really good point. Yeah. So I'm excited as the, the person who leads the research arm of arthritis and research advocacy, which is using data to drive legislative efforts or access to treatments that type of thing, which we've talked about here today. So that's my department. I'm really excited. So you would be at least a little bit I would be involved and helping you to learn how to do this. So we do like, like to say, whether the CEO or the newest volunteer, we're all equals y'all matter.
So I'm not distant just CEO. Okay. Well, yeah. That's a wrap for this episode of AiArthritis Voices 360, as we said, tune in for more research, more reports, updates. We've got dental, we have cardio, we have communication with your doctor, patient doctor relationships. Oh my goodness. Diagnosis struggles.
There's all kinds of things that we never even got to talk about today. But we have, we will be reporting back on them. You can find this episode and everything that all of the episodes at AiArthritis.org/talkshow. Please while you're at the website, consider a donation. We do a lot of work here that is not covered by grants.
And so we do rely on your donations to keep this going, including the research volunteer program that I just mentioned that is not paid for by any type of grant that is strictly going to be done with your gift. So please consider a donation AiArthritis so we can continue our research and including in the research databank.
Until next time, we do appreciate you and just remember, just because we leave the the table today, the conversation is not over. Please pull up your seat and together we can change the stories of tomorrow.
[01:06:25] Intro: AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www.AiArthritis.org. Also be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.
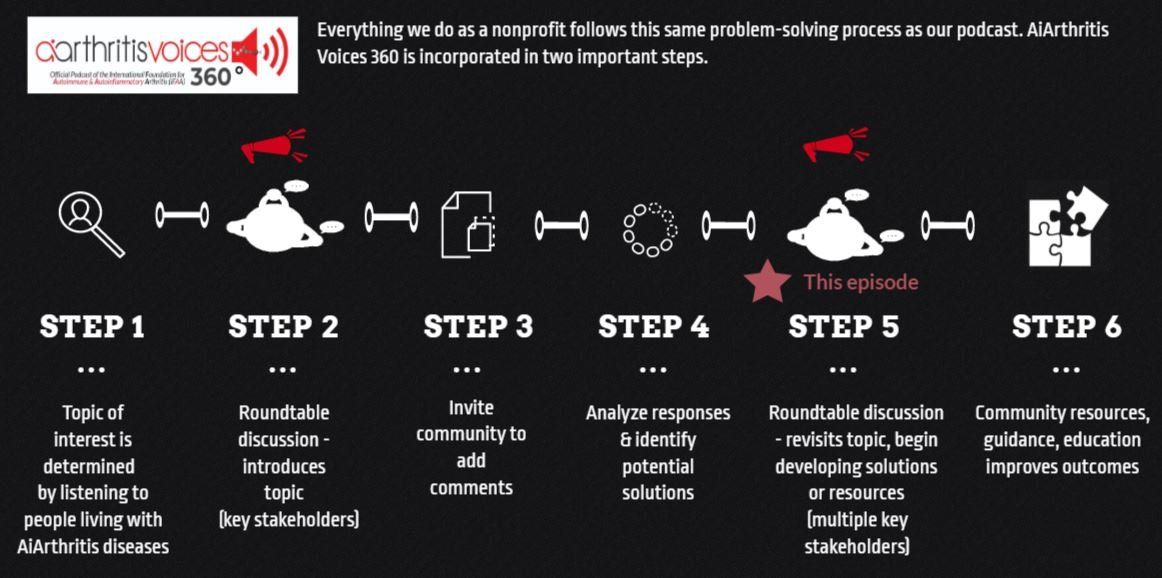
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!

And now, let's 360it!
The main Sunday episode is where we "put the topic on the table," but it's not where the conversation ends! Now we spin off the conversation into different discussion segments. Below you will find several 360its. Some are videos from the main episode, while others are audiograms (soundbites).
Soon we will be launching additional 360its, which will build on these conversations. We'll hear from patients in the United States, Canada, and Australia who are here to help you through the transition to biosimilars. We are also planning a WATCH PARTY, where we will play back segments of webinars that aim to teach you more about biosimilars - and you'll have your fellow patients at AiArthritis to talk through it all with you! Stay tuned.
360its & SHORT VIDEO CLIPS FROM THE MAIN EPISODE
#360it: Precision Medicine
Precision medicine is the key to unlocking tailored treatments for AiArthritis patients. As part of our podcast and #GoWithUs to conferences program, we delve into the importance of recognizing the uniqueness in each patient's journey.
#360it: Medicare Drug Price Negotiations: How Will It Affect Patient Access?
Join us in this breakout 360it from Episode 88 Biosimilars : Interchangeability & Switching 2023 as we dissect the Inflation Reduction Act (IRA) and its potential fallout on patient access to diverse treatment plans.
Your Host: Who is at the Table this Episode?
Tiffany Westrich-Robertson
Tiffany is the CEO at International Foundation for AiArthritis and uses her professional expertise in mind-mapping and problem solving to help others, like her, who live with AiArthritis diseases work in unison to identify and solve unresolved community issues.
Connect with Tiffany:
- Facebook: @tiffanyAiArthritis
- Twitter: @TiffWRobertson
- LinkedIn: @TiffanyWestrichRobertson
Deb Constien
Deb Constien is a medically retired Registered Dietitian and a Representative for the AiArthritis with Rheumatoid Arthritis. Deb is also on the Advisory Council for WREN- Wisconsin Research Education Network and a Patient Family Advisor- PFA on an International PCORI research study for ACP- Advanced Care Planning.
Connect with Deb:
- Facebook: @deb.majcherconstien
- Twitter: @debconstien
- Instagram: @debconstien
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Episode #74: EveryONE's Voice 'Precisely' Matters
In this episode, Tiffany, CEO of AiArthritis, is joined by Catherine Ames, from the Young Patients’ Autoimmune Research & Empowerment Alliance, both persons living with AiArthritis diseases and both who attended the 16th Annual Personalized Medicine Conference in May 2022.
Episode 36: Preparing Patients for Precision Medicine - Collaboration with the Rheumatology Nurses Society
In this episode, Event Host, AiArthritis CEO and person living with AiArthritis diseases, Tiffany Westrich-Robertson, is joined by patient Co-Host, Katie Steele. They speak with Carrie Beach, RN, from the Rheumatology Nurses Society (RNS) about our collaboration to improve patient voices in education and research (featuring our award-finalist Preparing Patients for Precision Medicine project).
Project: Advocating for Precision Medicine
While often the term "personalized medicine" and "precision medicine" are used interchangeably, AiArthritis differentiates the terms because we believe this will help advocate for access to biomarker testing, innovative treatments, and access to the right therapy at the right time for each individual OR subgroup.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.