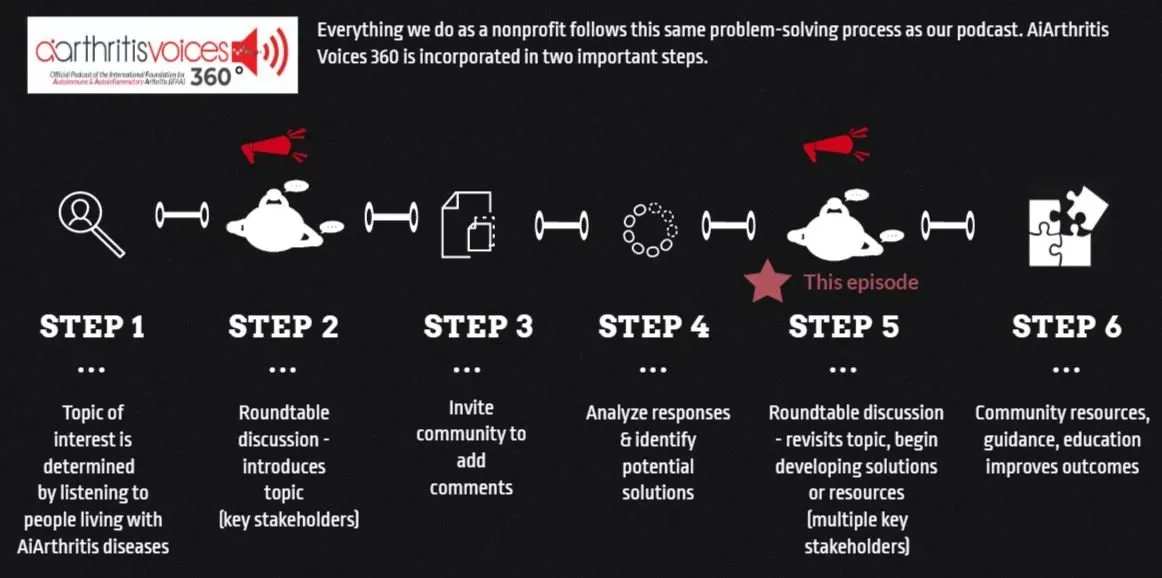
[00:00:53] Tiffany: Welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and Autoinflammatory Arthritis, or AiArthritis for short. My name is Tiffany Westridge-Robertson. I'm the CEO of the organization, but I'm also a person living with the diseases myself. My diagnosis is Axial Spondyloarthritis with a sprinkle of some other things in this autoimmune soup that most patients have.
And today, I am joined by some amazing experts that we're actually revisiting to the table today. We did an episode together last year on biosimilars, but some really urgent, important information for patients to understand is happening right now. And so we wanted to make sure that we came back to the table to tell you a little bit about it and keep you informed and also give you an opportunity to ask questions, more questions, and we will come back and give you answers as able, so the conversation does not have to end just because this episode does. So well let's meet our guests. So let's start with Michael. Michael, why don't you say hello and tell everyone a little bit about who you are and why you're here.
[00:02:08] Michael: Hello, Tiffany, and thanks for having me here today. I am the executive director of the Alliance for Safe Biologic Medicines, an organization that was started in 2010. So now 13 years ago, we were started at the Affordable Care Act, gave the authority to the FDA to establish a biosimilars pathway and we have been very active since then. Prior to that, I was in the Office of the Secretary at the U. S. Department of Health and Human Services, working for the Deputy Secretary, overseeing regulations both on the CMS and FDA side. And thanks again for having me.
[00:02:44] Tiffany: Great. Let's go next to Dr. McKibbin. Hello there.
[00:02:48] Ralph McKibbin: Hi, good morning, everyone. So I'm Dr. Ralph McKibbin. I am actually current chair of the Alliance for Safe Biologic Medicines, and I came to that organization through past experience. So I am currently on the Board of Governors of the American College of Gastroenterology, a practicing gastroenterologist, where I did practice management and work with different policy procedures and input.
I'm past president of the Digestive Disease National Coalition and still active in the group where we have an organization of about 40 stakeholders trying to come up with a synthesis of ideas and a consensus on policy and procedure to legislate and advocate on Capitol Hill and still on the board as an advocacy person and looking to negotiate with insurance companies and pass state bills, et cetera. And so I bring the physician stakeholder position and I hopefully those past experiences give me the language and the vocabulary to speak to other stakeholders, which is what I think we're doing here today. So I look forward to this discussion.
[00:03:47] Tiffany: Absolutely. Thank you. And last, but certainly not least, hi there, Andy.
[00:03:52] Andy: Hey, Tiffany. Thanks for having me. Yes, I also have been in the biosimilar space since the beginning. I co founded the Alliance for Safe Biologic Medicines with Michael and with other like minded patient advocates.
And so I am the stakeholder in the room representing the patient advocacy community. I've been very actively involved in the biosimilars landscape. As Michael said, we have either put on events or participated in events in countries all around the world and really have been the voice for biosimilar policy around the world through ASBM.
And my real job is the CEO of the Global Colon Cancer Association. There are many biologic medicines for colon cancer. And so it's, it's an extremely important area for us. We've seen the impact that biologic medicines have had both terms of life expectancy and side effect management and the real benefits of biologics.
And we wanted to make sure that as biosimilars have been rolled out over the last decade in the United States. And more broadly around the world, we wanted to make sure that the patient was at the center of all of these policy discussions. And so through ASBM, we really have been the voice with the WHO representing physician and patients, the voice at the FDA, the EMA all the way down to Australia, south America, central America. We have met with, certainly have a great relationship with Health Canada, really regulators around the world. And so Michael really did put together an, a meaningful organization that has made significant change around the world.
So really happy to be here and thanks for the invitation, Tiffany.
[00:05:42] Tiffany: Absolutely. And I, I'll second that kudos to ASBM. AiArthritis has been a proud member for quite a few years now and just do some acronyms for those who may not be familiar, Food and Drug Administration and European Medicines Agency.
So that's FDA and EMA. And I think it's very important to note as AiArthritis is an international organization, while we're going to focus on some issues here in the United States. We know that patients around the world, we all communicate on social media and support groups. So understanding this language is really important, no matter where you're living, because if we're communicating about our access or things that are happening, some of these words might come up.
And it's important for us, as we're communicating with each other to have a better understanding as well. Because it could become confusing if you live in different parts of the world. So we are going to jump right into this today. One of the main issues that we're going to zero in and the timing and why we want to do this is it's particularly in the United States that we have been able, well, largely through ASBM to be able to get 50 states to agree about interchangeability.
And I'm going to break out and have some other people explain exactly what interchangeability means is defined, but we've got buy in from this, right? And now it's being challenged and what does that mean for patients? What does that mean for doctors who want to feel confident in the safety and potential switching of a biologic to a biosimilar.
So we're going to get into all of that because it's really important to not only the patient community who's listening to this talk show, but we do have other stakeholder groups that also tune into this. So that's why we have so many stakeholders here today. So let's start by defining some things. So who would like to start?
We wanted to find biosimilar and then jump into switching and non medical switching to start. So who would like to kick us off?
[00:07:51] Ralph McKibbin: I can kick off the start of the discussion, and the first thing I want to just say as background is different people use the same words, and specialists often have a different definition in their head for what you're thinking, so I'm going to give my physician definition.
I think Michael can talk from the regulatory standpoint when we talk about interchangeable, etc. What's a biosimilar? If you have a medication such as adalimumab or infliximab, which is one of these biologic medicines for inflammatory chronic conditions, it's a living organism product, and you can't duplicate it exactly.
It's not made out of Legos, if you will. And so a different company can make something that's gosh darn very, very similar, very hard to tell apart and it does the same job. And so biosimilar is a medication that is almost exactly the same, a highly similar, if you will. And so it's tested and shown to have efficacy.
And so that's a medicine, it's not a generic. A lot of people use the word like that, but it's not exactly a generic, but as a practitioner, to me it's the same type of medications, I'm going to get the same result that's what I think it means. Switching is another definition to me that means if I write you a prescription or a plan of care, someone else, whether we agree to it or your insurance company or somebody is going to change things around.
So you may go in and as a patient in the United States, we have generic. So you may get automatic substitution and get that. It's been switched. So non-medical switching is when someone else decides, if I decide that's physician or patient interacted switching. Non medical switching is based on insurance company cost data, usually they want to limit the cost.
Automatic substitution then and this will tie into interchangeable, et cetera. I write you a prescription I don't put on their brand necessary or whatever your state equivalent is. You go to the pharmacy and they switch it out to something based on cost or whatever you choose to do, but many people will switch it around.
There are benefits to that for sure for cost. Sometimes there's issues in terms of agents in there. The classic is celiac disease. There may be gluten in some generics, but not in others. So you need to be careful with it. So then interchangeable from a physician standpoint, what does that mean? Means that I have been given the assurance that there's extra data that shows that your biosimilar isn't just highly similar, but we've done extra studies to show that there isn't any unsuspected side effects to a physician or practitioner, I shouldn't just limit it to physicians. Quality assurance, et cetera, is a process, not a thing. If you think of car safety, if you say a car is safe, is it safe forever? No, we have new standards that come along. I use the example of a renitidine and that NDMA contaminant. It wasn't in everyone, but we come along and say, Hey, let's pull that off the market because it's not what we thought it was. And so with biosimilars, the active ingredient is tested, but it's mixed in with other things, dissolving agents, etc. And so we want to make sure that this is truly staying the same.
And that extra data gives me the assurance that usually, and Andy can talk about this with his experience in advocacy, is that when you go to the pharmacy with your prescription or the infusion center, they may change it to something else because of that higher level of assurance without checking with me first. So, that's the physician definition of those words, and I think we can get some comments from the other folks too.
[00:11:29] Tiffany: Great.
[00:11:30] Michael: Yeah, and I'll just pick it up from there with regards to from the regulatory perspective as a former regulator and from the legislative perspective as someone who was a former Hill staffer.
First of all, the idea of interchangeable was really foresight by the Congress when they created the Affordable Care Act as an acknowledgement of the fact that biosimilars number 1, we were, we were behind Europe in terms of the start date. So they had an advantage on us. We have always been kind of compared to Europe, but they really were doing it multiple years ahead of us.
And so they did have the said start one of the issues with slower adoption, I think the Congress recognized, which was the need for additional data. Dr. McKibbin has talked about this and so has Andy. And so I think what Congress said is, if you can provide this additional level of data, you're kind of, it will take you more time on the front end to provide that data in order to get that approval status, but you'll make up for it on the back end because at that point, and this is where the state legislation came in. And that again was a nine year period to basically say at that point, you will have cut out a lot of steps, because we got the stakeholders to agree. And this is, I think, what they thought when it when when they passed the legislation that this an ideal world would happen and in fact, it did. And so they were simply trying to say to a manufacturer, if you want to take a little extra time, provide a little extra data, we will make it worth your while and ultimately that will lead to automatic substitution. So that's why the FDA said specifically you can automatically substitute a interchangeable biosimilar because we know it has provided an additional level of data.
[00:13:09] Tiffany: Great. Andy, did you want to add?
[00:13:12] Andy: I would say exactly what, what both gentlemen just said. I worked with ASBM with Michael, with the whole team for over a decade on the interchangeability issue. And I will tell you that it took a long, it took years to get all stakeholders on board and all 50 states and you know, I guess we'll be talking about that in a little bit, but I just wanted to say that the interchangeability issue for the patient perspective, if you're a cancer patient or you're an arthritis patient and your physician prescribes you a medicine, you know, we want that medicine, right?
And if we're going to agree, okay. from a patient perspective that a pharmacist gets to change our medicine that works at a hospital because it's saving the system money. If the pharmacist gets to change that medicine, there better be a good reason for it. And we better have reassurances that what you're going to change me to is safe.
And the fact is The selling point for getting all stakeholders to be on board for this was that interchangeability has a higher level of data standard requirement. And so by logic, they should be safer. So that's why
[00:14:32] Michael: I want to just clarify one thing, kind of piggybacking both on what Andy just said and what Dr McKibbin said earlier. Dr McKibbin talked in the beginning about how if you use the term generics with a biosimilar, it's not correct that basically there was an attempt early on to call them biosimilar generics or generic biosimilars. And that was rejected by really the scientific and regulatory community in recognition of the differences, that there are subtle differences.
Obviously, when you look at how in the states that have enacted legislation, all 50, with regards to interchangeable biosimilars and automatic substitution, they are treated as generics. So, obviously, the differences that you have brought them that much closer to the actual generic standard, and that's because of that additional data.
So to me, there's a attempt to kind of confuse by saying well, it's not a better biosimilar, you know, a generic or a interchangeable is not a better biosimilar. The FDA states that, by the way, it's not a better biosimilar, but the issue isn't a better or worse. The issue is whether or not you provided additional assurances to the physician, pharmacist, and patient community that you have data that tells you something that you otherwise don't know from the approval of a biosimilar, which is what happens when switches occur.
[00:15:50] Tiffany: No, you're absolutely. And we will touch on a few questions that our patient community had submitted as we go through this. And one of those main issues that we keep hearing over and over is when, especially when you live with these AiArthritis diseases, many of us have been through this trial and error, this grueling process of finding the right treatment.
And we have that history, we have that emotional connection to remembering what it was like to go through six months, a year, in my case, it was a year and a half to find the right combination treatment. So I'm thinking the word switch it means something to us. We get based on our emotional history, right?
So a lot of patients are still asking. I want to be reassured. I want to make sure that what the doctor feels confident. I want to make sure about the ingredients that are not the core ingredient, these dissolving agents, as Dr. McKibbin said, and that this assurance, a reassurance that there is the additional level of data.
And that's something that patients have really been asking for. So again, why this is so very, very important that we're talking about this right now. So we, we talked a little bit about all of these different definitions, And I wanted to specifically also ask for let me see here. I want to make sure I want to make sure with Michael here that there have been patients need to know specifically about these recent attempts.
And we're saying to muddy the waters on the concept of interchangeable biosimilars because interchangeable was defined differently elsewhere. So could you weigh in a little bit on that?
[00:17:41] Michael: Sure. So, like I said, I think from the beginning, and I mean, really early on, remember that our first biosimilar was approved here in 2015.
So, we're now 8 years into where we've had biosimilars and obviously more complicated biosimilars have been approved over a period of time. But from the beginning, when we were doing surveys across really Europe, Canada, even Latin America, and we were meeting with folks, there was this interest in the idea of interchangable biosimilar, and a recognition in different places that basically when they understood it was a, an additional level of data that, that had value.
At the same time, there has been to me, I used the word I think early on about an envy of that additional standard. There's always been a recognition that the FDA is the gold standard globally with regards to, you know, approvals in general. And I think the concern from listening to folks directly with the EMA, the Health Canada, they viewed it as kind of a negative because they thought ultimately it muddies the water for them with regards to the term interchangeable.
So they want to, if you use the term interchangeable and say all biosimilars are interchangeable, as in a doctor can take one product and switch it for another product. It's been approved by Health Canada, EMA, FDA. They're all interchangeable in that sense. But what we have always said, and I've often had Andy at my side, is that there is a difference between that term as it is understood in Europe in Canada and Latin America and Australia and the U. S. In the US it means it has gone through additional studies to demonstrate additional things and that is an important thing. Now, by the way, it doesn't always require and the FDA has made it clear. It doesn't always require switching studies, but it does always require the demonstration of what would be the equivalent of switching studies, in other words, being able to show what happens in the switch either way. And so to me, the first attempt to muddy the waters really started from the EMA last October, when they issued a statement, essentially saying all biosimilars are interchangeable.
And then they kind of doubled down on that in January to say, you know, almost like they put it out for public comment, but they really were just saying all biosimilars are interchangeable. I would say for patients interested in knowing what that means to go on the EMA website and there's a video on there that's about a minute and 50 seconds long that describes from the head of the EMA what it means to be an interchangeable biosimilar.
And they will understand that it is not what we were talking about with regards to interchangeable biosimilars, it is simply the ability to switch one for another. And again, they also make it clear that that is in most European countries directed by a physician. There's not a lot of automatic substitution in Europe, so there's a recognition of the fact that, you know, they don't want people to believe that a biosimilar is an interchangeable with another biosimilar in that way, but ultimately for us in the US, it means something different. On top of that, there's now an attempt at the state level and at the federal level, and there was just a bill that was in the help committee that got pulled until September to basically kind of one removes the ability for the FDA to demand essentially require switching studies to be a part of the designation of an interchangeable biosimilar.
That's ridiculous. I mean, the idea that you, and again, remember it's required, it means a manufacturer could still submit switching studies, but why would they, if they're no longer requiring switching studies and they can still get the designation of an interchangeable biosimilar. And by the way, and so doing completely undermines 50 state laws that were established on the basis of it being an interchangeable biosimilar.
To me, this is an attempt to basically drive uptake by changing the rules in the middle of the game, which is unfair to lots of stakeholders, including manufacturers, by the way, who have put the additional investment in, but most importantly, to the assurances that patients and physicians and pharmacists were given when they agreed to the legislation. I can tell you, not one state would have agreed to the legislation if it didn't include the word interchangeable biosimilar.
Number one, and number two, they all, it took us five years to get about four or five States on board. And then it kind of cascaded from there because everybody got on board and it was the initial stakeholders, you know, disagreements about a lot of different things. And so now you're basically saying, okay, well, we want to change the game.
We want to drive uptake. And the reality is that uptake is driven through confidence. And competition and confidence comes from additional data that Dr. McKibbin can talk to you about as a physician and Andy can talk to you as a patient and competition is competition. And certainly part of competition is a decision by a manufacturer to say, I'm going to apply and take the additional steps, provide the additional data and I know it's a long game because it will pay off both for us in terms of what we will be able to do in terms of automatic substitution, but also more importantly for the physician and patient community, because they have those additional assurances that mean they can turn their back when a substitution occurs and not worry about it as long as it involves an interchangeable
[00:23:00] Ralph McKibbin: Just to make a comment here and I go back to what I said that safety and whatnot is a process, not a thing. If you look at how healthcare has changed, we've added the patient voice as an example, as a prominent thing. You're supposed to be on decision making boards and pharmacy committees, et cetera, because those stakeholders were left out.
We have diversity and equity now in research, et cetera. It needs to be out there. This to me sounds like silencing voices so that we can just streamline it. And, and that's what we, I'm not saying we have to run it up the flagpole on every little thing, but gosh, let's have the discussions, not silence. And that goes back to changing the definition of terms.
Different people have different definitions from your side so I like the fact that there's that data, but that's the physician in me. And I think Andy talked about the patients, but we all need to sit at the table. And when those state laws were done, that's what we did to get them passed. Everybody agreed 50 states.
That's a big deal. And so the voices were there and why we're ignoring it just doesn't make sense to me.
[00:24:02] Andy: And Tiffany, I would add to that that the patient community was a stakeholder in all of these 50 state legislations. Frequently, it was me representing the colorectal cancer community and ASBM, but Arthritis was represented frequently.
Dermatology was represented and we, the stakeholder, the patient community bought in to this because of the higher level of scrutiny. We were going to say, it's okay for a non physician to change my physician's medicine based on the promise of more data. That's all. And so every stakeholder, including the patient community that bought into this, is being really slapped in the face by this proposed legislation.
You know, I don't know who these two people were that proposed this, but they certainly don't know better than the legislators of 50 individual states that had unique needs that had, you know, sometimes these bills had to be uniquely tailored. And sometimes the hearings that happened were last minute.
And we had to just jump on airplanes and go to state legislatures at the craziest times to get this passed. This was years of work. So I can't even imagine all of that being reversed without any good reason.
[00:25:24] Michael: I mean, I would say one thing about, he said, who is the bill? So the one bill is the Mike Lee bill, Senator Lee.
The bill is called the biosimilar red tape elimination act. If you can imagine that getting additional data is called red tape. It's really ridiculous that that is the name of it. And it's, you know, again, it's like you call a piece of legislation, something to appeal to a particular constituency, of course, but to say, and I can say this as having worked for six years in the office of the secretary.
To say that the secretary may not require additional data is probably pretty shocking to all of those people that were involved for all of those years to get this legislation passed in 50 States, as Andy said, it is a big deal and it took almost 10 years to happen and to simply say, we don't think it's going fast enough.
So we're going to try and speed it up and one of the ways we're going to do that is to begin to change the actual definition of what the FDA has done, rather than say, we now are getting a point where more interchangeables are being approved and let's just drive manufacturers to provide that additional data because then once they do that, that is an increase in competition, but it's also, you know, changing more people getting in and getting an enticing more manufacturers to give more data, to give more assurances to physicians and patients on the front end.
[00:26:52] Ralph McKibbin: You know, one other point here, and this is maybe just a comment to people who are watching this. We all have our way of looking at things, but regulators, patients and physicians very much understand and I'll echo what Tiffany said earlier when she was talking about her immune soup. There is a bell curve of disease, some people are very mild, some people are very severe. And when you approve a drug for Crohn's or Rheumatoid Arthritis, et cetera, they do studies, but it's a limited group, hundreds of people, perhaps maybe even thousands, but that's not millions worldwide.
And you have old and young and different conditions people with one immune disease have an 8% to 10% chance of a second. And so there's a lot of factors involved here and to say that all these patients are identical, they're widgets, you know, no, they're not. There are people with multiple needs and so we go back to that years of trying to get something right and to have it changed without even any input isn't right.
So I just for the regulators who see this, who don't understand patient care, that's part of the stakeholder value and why we're here today to echo that. And I just, we haven't talked about the patient voice in that respect. I wanted to bring it up.
[00:28:04] Tiffany: That's such a great point to bring up. Dr. McKibbin at AiArthritis, we are super invested in that subgroup that once a drug of any biosimilar or originator, when it comes to market, that it is designed in clinical trials for a segment of the population and that when we talk about value assessments or anything that's related in essence to access that we really have to consider what's happening with all of us. And that's why when we circle back to this whole issue with interchangeability is we as patients need to understand that this would, it's that same language, it's that same storyline.
We are not all the same. We are individualized and we do need to have that reassurance that this is something that our doctors, we're talking about, we have another layer of research behind that so we can feel confident because we know that the ones that came out in the clinical trials weren't necessarily reflective of us.
So thank you for bringing up that point. Andy, did you, I wanted to also let you weigh in a little bit because, you know, you have been really part of this landscape from the patient perspective as well. So is there anything that you wanted to add on to the whole conversation that just transpired?
[00:29:30] Andy: Honestly, if you just take the clip of everything Michael just said and just put that in a loop, it's everything that that he said that we're so concerned about you. It's so hard. I can't remember the last time I worked on any kind of legislation that that made it through all 50 states, you know, in a way that the patients were protected the whole time and you got all stakeholders.
We had, I remember when we didn't have all stakeholders, Tiffany, I remember in the early days, Michael, you'll remember the first four or five states. It was a fight with the patient groups on one side, payers on the other side.
[00:30:11] Michael: Well, and the physicians and the pharmacists, Andy, they didn't even agree.
[00:30:15] Andy: They didn't no, no, it was truly, it was truly, it was a mess in the beginning. And then we got language that everybody agreed on that we will promise patients taking this. We will promise physicians prescribing this and we will promise those dispensing this that if we allow this to happen, we will have higher levels of data.
And, you know, how do you, how do you go back on all those promises to all those communities, the physician, the patients, the payers, the payers were on board for this. It's on, it's unimaginable. And to go from where we were in the beginning of everybody's saying this is gonna break, this is gonna break us, this is gonna break us to consensus building was saying this does make the most sense for patients. This makes the most sense for those prescribing it and everybody was good with it. Just for example, the notification provision In the early days, the push on the other side was the pharmacist didn't want to notify the physicians that a switch occurred like it was something bad occurred. A switch occurred. We don't want to notify the physician that a switch occurred. And it was this whole crazy thing of this, this, this wrong perception that notifying the physician would be bad for a patient. And I'm standing there, the state legislature saying, could anybody explain to me how notifying my physician, if I'm a cancer patient, that a drug that he or she prescribed for me was changed by a pharmacist.
Who doesn't want their physician to be notified? Who doesn't want that to be part of the record? You know, all these issues had to be resolved in order to sell this to 50 states, and it all literally came down to, we can trust at a higher level being switched from one drug to another if they're switching studies done, if there's more data done, and that was the promise of this whole thing in every single state.
So it's almost every stakeholder that was involved in this movement, this decade long movement is just shaking, we're just shaking our heads saying this is a political thing has nothing to do with patients. It's in the worst interest of patients, and we just hope it dies quickly. That's my take on all this.
[00:32:35] Michael: Can I just jump in there
[00:32:36] Andy: And there's much bigger things we're worried about right now. So this shouldn't even, you know, be at the forefront. So go ahead, Michael.
[00:32:42] Michael: So I was just going to jump in and say, so to Andy's point, part of the issues, the things that went as parts of compromises in the beginning with regards to the whole idea of automatic substitution, remember important, I think, for listeners, we're talking about not to say one biosimilar is safe and one is not.
That is very clearly not what we're talking about. What we are talking about is the ability to make a switch from a physician prescribed without going back to the physician, that's a non physician directed switch. And that is something, by the way, that most of Europe doesn't even do. The physician is involved in most of the European switches that go on.
So that's the first thing. That was, in some respects, what we did here in the United States. Kind of like when a manufacturer goes through the additional data steps. It's a long game, right? It was a long game to say, we're gonna go, and we didn't know when we started we would ever get to 50 states. We didn't know that.
Really the issue in the beginning with the pharmacists and the physicians was physicians wanted advanced notification of a switch. They didn't want 72 hour notification. They wanted prior notification. And that was a big issue. And to defend the pharmacist on that, it was a matter of burden on how do you, you know, how is that possible?
How do you do that? We had the chairman of our advisory board, Dr. Schneider, who is a pharmacist testified, he's an Arizona pharmacist who testified against the Arizona pharmacist association on behalf of the bill to say you're being selfish, you need to look at the bigger picture and believe me, that was a big thing for him to do.
So the reality is, though, when you're talking about what this is, is a non physician directed switch that's different for patients. Tiffany, you mentioned it yourself. Andy can talk about the journey. At the end of the day, it is simply something that puts the U. S. ahead of the most of the rest of the world, except for those countries that don't really care.
You know, as I always say, there's a difference between Eastern Europe and Western Europe in terms of the issues that are that are that exist. Most of Western Europe has the physicians involved. I presented data from a European survey in 2019 that basically talked about to ESMO in Barcelona specifically showing that even though the confidence is extremely high with regards to biosimilars in Europe, across six Western European countries, they have a higher degree of interest in being in control of a switch and not allowing a third party switch than in the U.S. and that was well received there because in Europe they take pride in the fact that they have, for the most part, allowed physicians to be involved in the decision making. And they're, that's a best interest of the patient standard.
[00:35:29] Ralph McKibbin: Michael, to expand on that, you mentioned the surveys by ASBM, but if you look back at the surveys which are available on the ASBM website, the level of, physician's concern regarding switching and involvement has not gone down over the years that the studies have been done.
Well, each study is not exactly the same. The universal through it is that the physicians are still very concerned. In fact, probably more concerned than they were in the beginning. So this is a big stakeholder group who's very involved in the care, who still, after all these years says we need to be involved.
And I think that's a voice that needs to be listened to those surveys have meaning and should be looked at by regulators. Right.
[00:36:10] Tiffany: So what can patients do to stand up for these patient protections of this interchangeability standard that we've been talking about?
[00:36:21] Michael: Well, I think the first thing Tiffany is and I'll just there are multiple bills that we're talking about that are really an attack on it. There's the Lee bill. There's the help bill that just got pulled. There's a state bill in Louisiana that basically is trying to completely undo the work by saying that you can just literally insert the word biosimilar alongside interchangeable biosimilar and that completely eliminates the value of an interchangeable biosimilar.
And so what I expect, and I've been kind of predicting this for a couple of years, that you're going to start to see this at the state level. The best thing for your organization, certainly what ASBM is going to do, is to be very mindful of the bills as they pop up to make sure that we gather signatures and put together letters in opposition in those legislation, and the reality is we're on the right side of this issue. This is an attempt again to drive uptake and to completely change the rules. And by the way, the standard was established by the FDA. The FDA it took them years to figure out how to go and you know, without overburdening manufacturers to the point where you couldn't apply as an interchangeable biosimilar.
And now they're getting momentum in that regard. And so why would you now change all of that? That's the odd part about it. It's strictly about uptake. And frankly, I think it started with the EMA's statement last October and going into January where they were just trying that statement had ramifications here in the U. S. it wasn't just for Europe. It was to basically say, we think all biosimilars are interchangeable, but it's really word, you're just playing with words. Because again, if you look at what the EMA says about it in that video, it has nothing to do with what we're talking about. It has to do with, can Dr. McKibbin switch a patient him in charge, can he switch a patient? And he certainly knows he can. But he wants to be involved.
[00:38:18] Ralph McKibbin: You know, one other thing about being involved in this process of advocating is we haven't talked about pharmacy benefit managers. Different from Europe where perhaps they have a single contract etc over here we have multiple payers and there's a drive for instance in Pennsylvania now we have bills for transparency and auditing pharmacy benefit managers and contracting so they can see what's going on because what are we talking about here?
We want to change to a biosimilar because it's going to supposedly save money, but save who money, or is it increased profits, et cetera. We want transparency in the process so that all stakeholders can look at the data and say, oh well, let's do it the right way with this data shows. And when you have carriers and insurance companies not disclosing what they're doing or how they're making decisions, it's important.
So I would just say that. Patients need to advocate like in Pennsylvania. We have these transparency laws out there on pharmacy benefit managers because the pharmacy benefit manager often owns the insurance company now, et cetera. And so the pharmacy and therapeutics decisions are much more complicated here as opposed to, say, a single payer contract say in the EU, where you pick the best contract. It's a little more complicated here, and we need that transparency and advocacy. So I would say, what do you do? Be the squeaky wheel and get your voice out there through decisions like this and your organization.
[00:39:45] Tiffany: Absolutely. Andy, did you? Oh, I'm sorry. Go ahead, Michael.
[00:39:49] Michael: Just one more thing I wanted to point out is that I mentioned in the beginning how the EU, EMA and Health Canada were, I use the word envious, but basically kind of looking at the idea of an interchangeable biosimilar and saying this kind of complicates things for us.
What I didn't mention is I also met with the Department of Health in Australia who are having their own challenges around automatic substitution. And when they began to basically allow for automatic substitution, but in order to assure the patient and physician community, they allowed physicians to basically opt out, thinking that the physician would not opt out, meaning tick a box and basically say, do not substitute.
And over 95% they actually ticked the box. They took the extra step to not substitute. And that was because of lack of data and confidence. When, when I met over with the department of health and we met with the rheumatology organization in Australia, who was really leading the opposition to this automatic substitution concept.
I said to them, I talked to them about, you know, as a former regulator, the idea of interchangeable biosimilars. And I said, there's no reason why Australia could not simply say, we will accept all interchangeable biosimilars that are approved by the FDA as interchangeable here in order to basically help expedite the problems that they were having and they like that idea.
Now, they haven't acted on it. So I don't want to overstate it, but they definitely and that's because it's a big difficulty to be able to do that. But in terms of conceptually talking about it, They understood that the stakeholders pushback in Australia, which is well documented, was because of that additional data, and they recognized the value of an interchangeable biosimilar, and that if they had something similar there, they would be way further ahead, and it took them years to really begin to push through and get substitution levels there because of the opposition of the, of the physicians and patients in Australia.
[00:41:50] Tiffany: Thank you for that. Andy, did you want to add anything also from patient's perspective or things that you all are doing that we can join collectively as well?
[00:41:59] Andy: You know, just dovetailing off what Michael said in the Australia thing, from what I recall, didn't they do, I think it was called a flogging, Michael, where a flagging where the physicians basically revolted, didn't they? And they had no uptake of biosimilars. They were writing, do not substitute, right, on every prescription.
[00:42:21] Michael: And those decisions were driven by budget projections that they had promised savings in their budget. And they did not materialize because, again, they, the optics of it were, well, we're going to let the physicians opt out if they want to, and that will give you the assurances that they're involved in the decision.
They never expected that the physicians at the level they would, would take that additional step. They figured that if you make them have to actually do something additional, they will just let it go through and it would be automatically substituted. It didn't happen. The substitution happened at a less than 5% level, which meant the physicians felt very strongly about it.
And again, it goes back to this whole conversation
is about trying to move forward the whole biosimilar paradigm. We have advantages that are built in, in the U S. In the in the foresight of Congress, when they gave the ability of the FDA in the time it took for the FDA to get it right to figure out what additional data not too much.
It's literally a situation where they said we don't want to overburden because we want to make sure we can get them approved because there's a value in that. But we also want to give assurances. And so we are ahead of the rest of the world with regards to the value of an interchangeable biosimilar.
And you will notice that the only attempts to undermine that are not by regulators. They are by legislators who are, who are focused on budgets. They're not focused on policy. They're not focused, they have no understanding of how the process that we've all been describing took place and the years that it took to get the agreements that it did.
And it is actually a complete disregard for the patient, physician, pharmacist, all the stakeholders that were engaged in this conversation because it was years of negotiating to say, okay, I want this, but I'll take that and let's move it forward. And the momentum really began to grow. And now you've got interchangeables coming out.
I, I just find it incredible that you would, you know, I, I don't, I can't even find a value in doing it other than basically to just bypass the current system and say, you know what? We think automatic substitution is a great idea and we don't really care about what's being automatically substituted.
[00:44:31] Tiffany: All right. Well, we're going to, we're going to jump into some patient questions that were submitted and intertwine the conversation that we're having into answering them because you'll see as I ask those questions, this is all very, very relatable to the conversation that we're having. So one of the questions that came in prior was what are the chances of failure on the original biologic if you fail on the biosimilar and go back to the original, they wanted to know what studies were being done on that.
And the reason that this particular question. It was submitted in several different formats is important is because it's really expressing the concern of the patient for data to understand, is this going to work for me? So, Dr McKibbin, could you maybe weigh in on experiences with non medical switching and assurance or what this interchangeability means for patients who ask this particular question?
[00:45:34] Ralph McKibbin: So have studies been done on switching? Yes, they tend to be small. Let me just back up and just say when a biosimilar is presented or created, they will do studies that show, I'll use concrete examples, that it works for Crohn's or Rheumatoid Arthritis the same, and then they extrapolate that it will work then for all the others, and they're not necessarily studied for those other diseases.
And so they'll, they've done some small switching studies in different places, and there is a background rate of failure, but there's a rate of failure anyway. People who were on a medication for years will sometimes You know, stop working. So there isn't a higher rate of failure. But anecdotally, I can say myself, I've had four patients who were stable for years who failed their biosimilars this year when they were automatically switched.
Not automatic. I shouldn't say that when they were switched and they agreed to the switch, but they were infusion medicines. So the data isn't there. We don't have registries. That was one of the things that physicians had advocated for that at least we could do a post marketing thing and do registries this data really aren't there and they tend to be isolated.
For instance, they might do one in Scandinavia, Norway or something like that. And that's a not all patient groups are there, not all ages and racial groups, etc. So the data aren't universal. There is no big data and so it's still an ongoing concern. But I think we inherently believe that biosimilars work and they do, and we have a level of trust with it.
But no, there aren't studies going on to keep this going forward. Does that answer your question? I think,
[00:47:16] Tiffany: Yeah, it does.
[00:47:17] Michael: And Tiffany, could I just, can I just add on to that? Because the expression I use as I go around as a former regulator meeting with physicians and then with regulators is the absence of data is not data.
And that is really what the challenge has been around biosimilars. It has been by those who are saying, show me data that shows that there's failure. Show me data that shows that there's adverse events. Show me data that whatever. And so our response has always been the absence of data isn't data. It's the same, it's, it's still an absence of data. That's why interchangeable biosimilars are so helpful for physicians because that's actually the presence of data, right? And just one more thing that he mentioned, Dr. McKibbin has mentioned, we had a meeting in Canada where a Norwegian regulator presented to this group in Ottawa and talked about the fact that when the tender system was done in, in Norway, the, they asked the winner of the tender. So they win the tender and they now have the entire market and they asked them, well, can you provide data as a result of the winning of the tender? And they said, well, the manufacturer said no.
And so what I said to the regulator is why is that not a condition preceding that if you win the tender, you provide the data that should be a condition upon winning the tender, because it struck me for years, you would think that there would be a lot of incentive for multiple manufacturers to be by now we'd have a lot of data.
If a lot of data was gathered that could be provided, and instead it's still this elusive show me that there's data to prove otherwise, instead of you could have gathered just in the States alone, eight years of data from the use of biosimilars.
[00:48:55] Ralph McKibbin: One of the things about switching is we always look at the pharmacy cost.
But if you look at adverse effect studies, it's cost to the system. So non medical switching has been shown to raise costs, hospitalizations, adverse events, et cetera, doesn't necessarily change the pharmacy numbers. And so when they bid these contracts are saying we can save you money at the pharmacy or on the cost of drugs, but they don't carry the data to the other side and show you that the system costs are higher. But those studies have been done. I was lead author on a white paper for the Digestive Disease National Coalition, where we reviewed non medical switching, and how the adverse effects were there. So the data is there, and I agree with Michael, there should, especially in a country where you have one, everybody's on the same thing, there's big data, boy, wouldn't it be a service to the world to show whether it was working or not?
[00:49:48] Tiffany: Absolutely. One of the things I also wanted to tie in, it was a patient question, and it really is relevant to this whole interchangeability. In retrospect, they asked, and you had alluded to this, Dr McKibbin, in the very beginning, that one of the top things that patients are concerned about and why they would be more confident with something that's interchangeable is they are worried about the additives.
They're worried about how things were formulated and they want to know, do they have to be concerned about this with biosimilars, especially if they're going to be switched without, without their doctors saying, yes, I think this patient should be switched, especially if they have a history of having reactions.
[00:50:33] Ralph McKibbin: So there are definite issues there and adalineumab, is an injectable used for Crohn's, rheumatoid, et cetera. And initially it had citrate in it, citric acid, which burned when you injected it. They've since come out with a citrate free formulation, which is much more tolerated, but there are biosimilars that have the citric acid in it.
And people wouldn't, you know, the best medicine is the one you use. And so if there's a pain with injection and swelling, people may not want to use that. Also for injectables, the syringes themselves, the auto injectors may not be the same. So if you have bad arthritis, you may not be able to use it. So those are real factors as well.
It's not just the active ingredient. And maybe this is a time to talk about the ophthalmic data, the Canadians auto substitution. But Ophthalmologists are just really beginning to use biologic medicines, and they inject them directly into the eye, and so some of the biosimilars have dissolving agents, or excipients is the big word, but they may not even be approved for use in the eye, and so they're being told to use a biosimilar, but yet the ingredients in there are not approved for eye use, and so they have a lot of concerns, and our ASBM survey shows that there's a high level of concern, similar to all the other physician groups about being able to deny, et cetera.
So is it an over concern? No. I mean, I think people have used these, the excipients used in the biosimilars for the most part work. However, I go back to what I said about celiac. Sometimes there's something you can react to. Remember, if you look at that bell curve, the people at the mild end don't have any opinion for the most part.
I think that, you know, they're not bothered by this. It's the people at the high end who are the most complicated, but also the most expensive that are driving this, and they need to put their voice out there. So, yes, you can have adverse reactants. And it needs to be that's what you work with your physician for, you know, and, and we may not even know what's there, but we know that if you have had problems that we would want to switch you back, etc.
So it's the high end complicated patients who should have the biggest concern. I don't think anxiety. But concern, you know, the squeaky wheel gets the grease and speak up.
[00:52:52] Tiffany: So we are at time and winding down. So I wanted to just throw it back out on the table and ask each of you, if there's a very important takeaway that you would like to wrap up here and sort of your summary of what our audience really needs to understand what would that be? Dr McKibbin, would you like to start?
[00:53:14] Ralph McKibbin: Well, I think putting my different hats on. I think my takeaway is to speak up and be part of the decision making process. We talked about laws being passed and stakeholders and representation. There is data out there, and that was one of the reasons that Digestive Disease National Coalition white paper was written.
People complain about things, but you feel like maybe you're just complaining, and the fact is there is data. So I always said if you thought of it as a comic book, there's writing and there's illustrations, and the patient stories are the illustrations of the points that we're making, and that's what influences our legislators, etc.
So speak up, advocate, get the words out, and get more programming, and then send links to your representatives. I think, I think, you know, we can't just be an advocate for yourself. That's my, my message.
[00:54:04] Tiffany: All right. Thank you for that. Michael?
[00:54:07] Michael: Looking at this whole conversation and most of it focused around interchangeable biosimilars if it ain't broke, don't fix it is kind of what I would say about it.
The reality is there was a lot of wisdom in creating the interchangeable biosimilar. There was a lot of work in building off of that wisdom and that creation, and that is at the state level. And there really is no advantage that you could see to changing the system other than just shortcutting it.
And so from my perspective, you know, as I tell people as a former regulator and having worked on the Hill, just because someone's trying to pass something doesn't mean it's a good idea. And I would just say with regards to the types of bills that we're talking about, whether it's the Louisiana bill. Or whether it's the two federal bills, they are attempts to basically circumvent a process that had one goal in mind, and they're trying to do it for a completely different reason.
The goal of setting up interchangeable biosimilars was to give multiple stakeholders, manufacturers, an opportunity to invest more, and hopefully it would pay off in terms of the assurances they got that results in market share, that results in Their ability to market their product, frankly, as a product that is, that is, you know, again, back to this conversation of whether it's better or not better, that's up for the consumer to decide.
And in some respects, they have decided by passing legislation in 50 states to treat it differently. So that's not about better or not better as to the efficacy and safety. Those are different issues. But with regards to the necessary assurances that allow Dr. McKibbin to deal with another patient and not worry about what happened to that patient knowing that he's already signed off on the process is really important and it should not be changed. And we at ASBM will do everything we can to make sure it's not.
[00:56:00] Tiffany: All right. Thank you for that. Andy?
[00:56:03] Andy: Well, again, everything's been said before me. It's perfectly said. So there's nothing really to add to that, except I would say that to add to it ain't broken, don't fix it as Michael said, there's no issue out there. There's no urgent issue that this legislation is addressing. The U.S. biosimilar's experience so far has been a success story by every metric. We are probably outpacing Europe, who had a decade of experience before us. When you do, I don't know, Michael, you may have this data, you know, off the top of your head, but I know I've seen the data presented that the US success story with the number of biosimilars have been approved and the amount of time that biosimilars have been here in the US, we're outpacing Europe in terms of approval in that length of time. And the projection is that we're going to actually outpace Europe very quickly. It's a success story in every metric.
[00:57:08] Tiffany: So to, to wrap this up, as you see, there's a lot to talk about here. And that's why we will continue the conversations in many ways.
So we will make sure that all of the links that we mentioned or in association with the groups that are presenting here are part of our panel today will definitely be included and the IRA webinar that was on the other day when that recording is available we will also have that as well and I attended that so I can attest it was very informational.
We want to make sure that the conversation doesn't end here. So you can always continue this conversation as we post about this episode on all of our social media channels, which is at IFaiArthritis. So that's on all the same on all of them. You can also, if you would like to submit your questions, concerns, comments, you can go to AiArthritis.org/biosimilars. And we have a hotline right there. Just push the button and you've got patients on the other end who are reading those. And then while you're on there, you could also sign up for our newsletter and specifically check advocacy that way we can follow up with you on all of these efforts that we will be doing to make sure that your voice is heard. And while on there as well, you can certainly find this and all of our episodes and 360its on our site as well. So thank you all our guests today. And as I said, the conversation won't end just because this episode does. So thank you all for joining us.
Until next time, thank you for coming to the table.
[00:58:45] Ralph McKibbin: Thanks, Tiffany.
[00:58:46] Michael: Thank you.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www.AiAirthritis.Org. Also, be sure to subscribe to this podcast. And stay up to date on all the latest AiArthritis news and events.
Introduction